Glaucoma
Use IOLs with Caution
Presbyopia-correcting IOLs in glaucoma patients involves a multifaceted decision.

Cheryl Guttman Krader
Published: Thursday, March 2, 2023
“ Glaucoma has been considered a contraindication for using a presbyopia-correcting IOL; however, this is controversial because high-level evidence is lacking. “
For patients with glaucoma seeking reduced spectacle dependence after cataract surgery, offering a presbyopia-correcting intraocular lens (IOL) should be on a case-by-case basis taking into account multiple patient- and IOL-related features, advises Filomena Ribeiro MD, PhD.
“Cataract and glaucoma often coexist, and patients with both conditions are seen with increasing frequency. Glaucoma has been considered a contraindication for using a presbyopia-correcting IOL. However, this is controversial because high-level evidence is lacking,” said Professor Ribeiro.
“Multifocal IOLs should be used with caution in patients with glaucoma but perhaps considered in those with early, stable disease with a low risk of progression. Other IOL options can provide patients with more functional vision.”
Careful preoperative evaluation
The decision to implant a presbyopia-correcting IOL is partly guided by whether the preoperative examination identifies issues with the potential to affect functional outcomes. Attention should be paid to the ocular surface condition, recognising that dry eye is common in glaucoma patients. The examination should also look at structural features of the anterior segment that can be affected, including anterior chamber depth and symmetry, as well as the irido-corneal angle, pupil, and iris.
In addition to the stage of glaucoma, surgeons should examine the possibility a multifocal IOL can affect interpretation of tests used to monitor glaucomatous progression and the potential for disease development following cataract surgery. Without these considerations, the risk increases for glaucoma progressing to a point requiring filtering surgery that can induce astigmatism, or a patient with pseudoexfoliation glaucoma could develop zonular laxity that will affect IOL stability.
Evaluations should also include visual function measurements to determine if the patient would benefit from a multifocal IOL or suffer relevant compromise due to existing reduced contrast sensitivity. Noting visual acuity is not a good indicator of visual function in patients with early glaucoma, Prof Ribeiro said the evaluation should rely more on contrast sensitivity, with mesopic the most relevant.
“We know contrast sensitivity is compromised even in patients with ocular hypertension and early-stage glaucoma, and published studies show contrast sensitivity with and without glare is worse after implantation of a diffractive multifocal IOL than a monofocal IOL,” she said. “However, [studies also show] contrast sensitivity in normal subjects over sixty years old is not that different.”
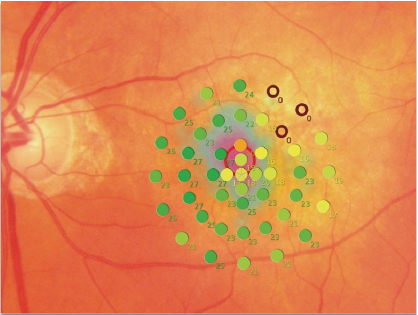
Central retinal sensitivity will determine whether a patient will benefit from a multifocal IOL. Furthermore, mean deviation values are reduced by multifocal IOLs, although there is a lack of information on the effects of newer trifocal and EDOF designs.
Prof Ribeiro noted microperimetry’s use in assessing the central visual field. It has also shown strong correlations with structural parameters obtained by OCT and offers slightly better reproducibility.
“Of course, [microperimetry] is not the perfect examination. In the future, new functional assessment methods can complement structural information provided by OCT,” she said.
Multifocal alternatives
Prof Ribeiro suggested newer enhanced monofocal IOLs might be an option for giving patients more functional vision for daily activities without further reducing contrast sensitivity. An add-on multifocal IOL that can be explanted in the future, leaving the patient with an in-the-bag monofocal lens, is another possibility.
“We do not yet have evidence to support this approach, but it is being studied,” she said.
Prof Ribeiro spoke at Glaucoma Day during the 40th Congress of the ESCRS in Milan.
Filomena Ribeiro MD, PhD is the Head of the Department of Ophthalmology, Hospital da Luz, Lisbon, Portugal. filomenajribeiro@gmail.com
Latest Articles
From Lab to Life: Corneal Repair Goes Cellular
Long-awaited cellular therapies for corneal endothelial disease enter the clinic.
Balancing Innovation and Safety
Ensuring access to advanced cell therapies amid regulatory overhaul.
With Eyes on Its Future, ESCRS Celebrates Its Past
Winter Meeting offers opportunities to experiment with new concepts and formats.
Best of ESCRS Winter Meeting 2024
Following the New Generation
EDOF IOLs an option for eyes with mild comorbidities, showing potential in mini-monovision strategies.
Refocus on Multifocals
Trifocal IOLs continue to improve as consensus grows regarding indications and contraindications.
Common Myths in Presbyopia Correction
Patient education key to satisfaction with refractive IOLs.
Reversible Multifocality
Two-lens combination offers low-risk spectacle independence for cataract patients and presbyopes.
Managing a Cataract Surgery Refractive Miss
Weighing the pros and cons of options for intraocular intervention.
Unleashing OCT’s Full Potential
Performance of newest tool for corneal evaluation meets or beats older standard technologies.