The threat of herpes in ocular surgery
Prevention of herpetic reactivation essential in at-risk patients undergoing corneal surgery

Roibeard O’hEineachain
Published: Monday, April 1, 2019
[caption id="attachment_14423" align="alignleft" width="1024"]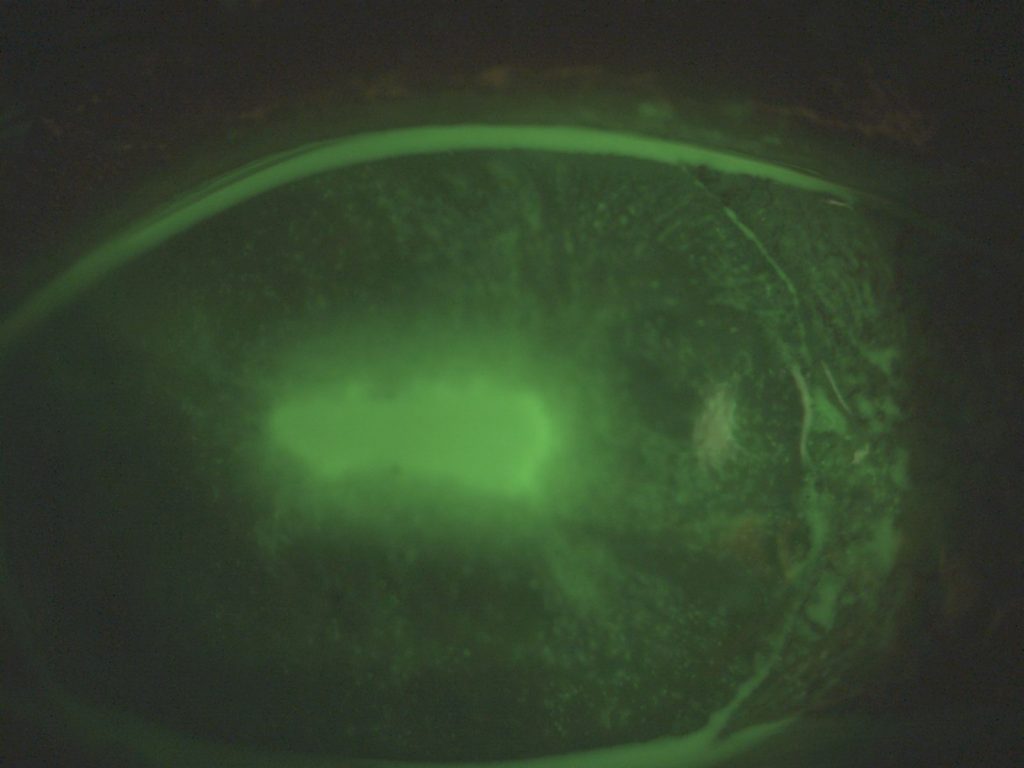 Example of geographic keratitis observed four days after cataract surgery in a patient without previous history of herpes simplex ocular disease[/caption]
Ophthalmic surgeons should take precautions in eyes with a history of herpes simplex keratitis (HSK) and herpes zoster ophthalmicus (HZO), said Marc Labetoulle MD, Bicêtre Hospital, Paris France.
Example of geographic keratitis observed four days after cataract surgery in a patient without previous history of herpes simplex ocular disease[/caption]
Ophthalmic surgeons should take precautions in eyes with a history of herpes simplex keratitis (HSK) and herpes zoster ophthalmicus (HZO), said Marc Labetoulle MD, Bicêtre Hospital, Paris France.
 Marc Labetoulle MD
Speaking at the 23rd ESCRS Winter Meeting in Athens, Dr Labetoulle noted that surgery involving the cornea brings with it several triggering factors for the reactivation of HSV and HZO, including nerve trauma, steroids, and inflammation.
He noted that almost everyone is a candidate for HSV or varicella zoster virus (VZV) reactivation, since 90% of 50-year-old people have antibodies to HSV and VZV. The presence of the viruses in the trigeminal ganglion is 80% at 20 years of age and 100% at 60 years, even in a few patients without antibodies.
The lifetime risk of herpes zoster is 10-to-20% and that is multiplied 15 times in HIV-infected patients, where the recurrence is 25%, versus 4% in immunocompetent patients. As HZO accounts for 10-to-20% of all herpes zoster infections, the lifetime risk of HZO is 1-to-4%. Concomitantly, the lifetime risk of herpes simplex keratitis is 0.23% by 30 years, 0.4 % by 50 years but 0.94% by 80 years.
Risk factors for reactivation include physical factors such as ultraviolet radiation, cold, ocular surgery such as keratoplasty, refractive and cataract surgery, corneal cross-linking and iris laser surgery. There are also biological triggers including immunosuppressive treatments, ophthalmic solutions containing steroids, fever and general anaesthesia.
He noted that HSK-related disease is a major indication for corneal grafting. In a series of 2,962 grafts HSV accounted for around 10% of cases. HSV is also a major cause of graft complications. In addition, the risk of HSK recurrence following a corneal graft is 25% at one year and 45% at two years.
Meanwhile, cataract surgery carries its own set of risk factors for HSV reactivation and corneal nerve injuries as it involves a combination of several risk factors, including stress and fatigue from early waking and postoperative inflammation. Other contributing factors may include preoperative eye drops such as preoperative alpha mimetics and postoperative steroids.
It is vital, therefore, to check the HSV and VZV status of all patients when planning corneal or cataract surgery. Patients at risk should receive prophylactic treatment with antiviral medication such as acyclovir or famciclovir at least two days before the procedure and the treatment should be prolonged at least as long as postoperative steroid treatment.
He added that only systemic treatment is logical in such cases. Research indicates that the recurrence rate, in the case of corneal graft, is only 12% with systemic treatment, compared to over 50% with topical treatment. In addition, the rate of graft rejection is 52% with topical treatment compared to 20% in systemic treatment.
Practical recommendations when dealing with patients with a history of herpes simplex keratitis or HZO include delaying cataract surgery by three-to-six months and using systematic antivirals, starting two days before surgery and as long as risk factors persist and at least as long as the patient is receiving steroids.
Dr Labetoulle cautioned that antiviral prophylaxis is not without risk. For example, in patients with idiopathic thrombopenia the antivirals can decrease platelets to dangerous levels. In patients with pre-existing renal failure, the dosage must be adapted to creatinine clearance. They can also disturb liver function. He also noted that they don’t prevent all recurrences as some HSV variants have mutations that result in a selection of resistant viral strains.
In patients with a history of HZO, surgeons should also be on guard against post-viral keratitis. Assessment of corneal sensitivity is therefore mandatory to detect potential neurotrophic keratitis. Corneal perforation can occur in eyes with the condition when NSAIDs are used.
He added that thankfully in the future HZO will probably become less common with the advent of the varicella zoster vaccine. It should reduce the number of cataract candidates who have already had a herpes zoster infection and also reduce the risk of recurrent episodes of recurrent inflammation.
Marc Labetoulle: marc.labetoulle@aphp.fr
Marc Labetoulle MD
Speaking at the 23rd ESCRS Winter Meeting in Athens, Dr Labetoulle noted that surgery involving the cornea brings with it several triggering factors for the reactivation of HSV and HZO, including nerve trauma, steroids, and inflammation.
He noted that almost everyone is a candidate for HSV or varicella zoster virus (VZV) reactivation, since 90% of 50-year-old people have antibodies to HSV and VZV. The presence of the viruses in the trigeminal ganglion is 80% at 20 years of age and 100% at 60 years, even in a few patients without antibodies.
The lifetime risk of herpes zoster is 10-to-20% and that is multiplied 15 times in HIV-infected patients, where the recurrence is 25%, versus 4% in immunocompetent patients. As HZO accounts for 10-to-20% of all herpes zoster infections, the lifetime risk of HZO is 1-to-4%. Concomitantly, the lifetime risk of herpes simplex keratitis is 0.23% by 30 years, 0.4 % by 50 years but 0.94% by 80 years.
Risk factors for reactivation include physical factors such as ultraviolet radiation, cold, ocular surgery such as keratoplasty, refractive and cataract surgery, corneal cross-linking and iris laser surgery. There are also biological triggers including immunosuppressive treatments, ophthalmic solutions containing steroids, fever and general anaesthesia.
He noted that HSK-related disease is a major indication for corneal grafting. In a series of 2,962 grafts HSV accounted for around 10% of cases. HSV is also a major cause of graft complications. In addition, the risk of HSK recurrence following a corneal graft is 25% at one year and 45% at two years.
Meanwhile, cataract surgery carries its own set of risk factors for HSV reactivation and corneal nerve injuries as it involves a combination of several risk factors, including stress and fatigue from early waking and postoperative inflammation. Other contributing factors may include preoperative eye drops such as preoperative alpha mimetics and postoperative steroids.
It is vital, therefore, to check the HSV and VZV status of all patients when planning corneal or cataract surgery. Patients at risk should receive prophylactic treatment with antiviral medication such as acyclovir or famciclovir at least two days before the procedure and the treatment should be prolonged at least as long as postoperative steroid treatment.
He added that only systemic treatment is logical in such cases. Research indicates that the recurrence rate, in the case of corneal graft, is only 12% with systemic treatment, compared to over 50% with topical treatment. In addition, the rate of graft rejection is 52% with topical treatment compared to 20% in systemic treatment.
Practical recommendations when dealing with patients with a history of herpes simplex keratitis or HZO include delaying cataract surgery by three-to-six months and using systematic antivirals, starting two days before surgery and as long as risk factors persist and at least as long as the patient is receiving steroids.
Dr Labetoulle cautioned that antiviral prophylaxis is not without risk. For example, in patients with idiopathic thrombopenia the antivirals can decrease platelets to dangerous levels. In patients with pre-existing renal failure, the dosage must be adapted to creatinine clearance. They can also disturb liver function. He also noted that they don’t prevent all recurrences as some HSV variants have mutations that result in a selection of resistant viral strains.
In patients with a history of HZO, surgeons should also be on guard against post-viral keratitis. Assessment of corneal sensitivity is therefore mandatory to detect potential neurotrophic keratitis. Corneal perforation can occur in eyes with the condition when NSAIDs are used.
He added that thankfully in the future HZO will probably become less common with the advent of the varicella zoster vaccine. It should reduce the number of cataract candidates who have already had a herpes zoster infection and also reduce the risk of recurrent episodes of recurrent inflammation.
Marc Labetoulle: marc.labetoulle@aphp.fr
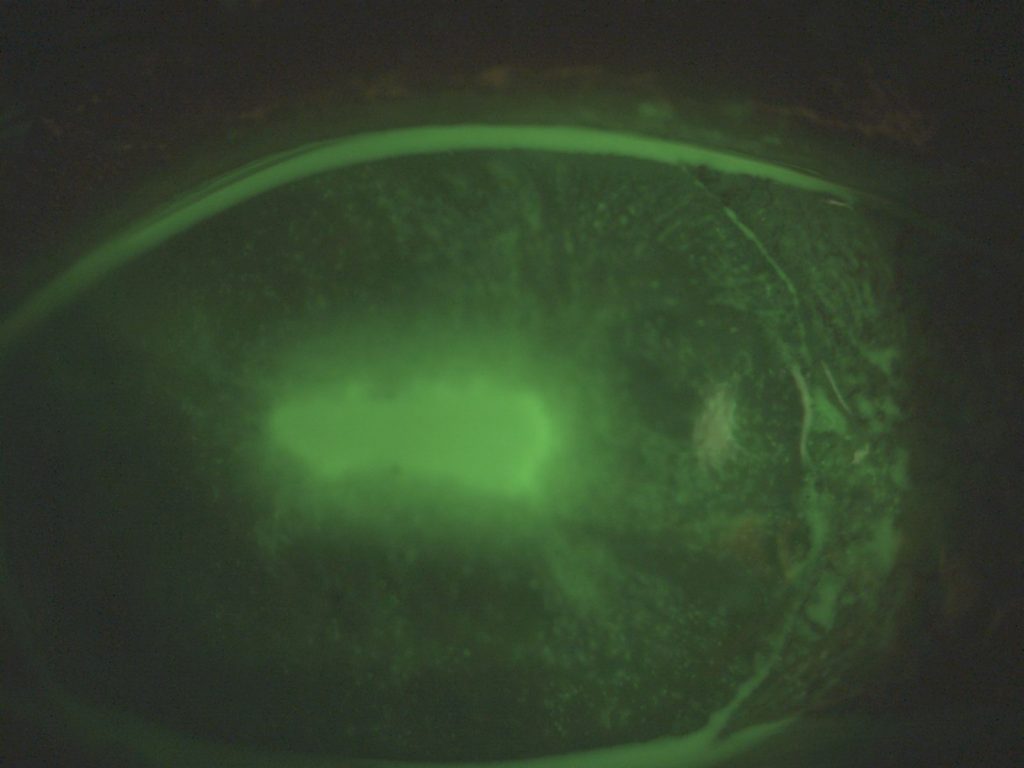 Example of geographic keratitis observed four days after cataract surgery in a patient without previous history of herpes simplex ocular disease[/caption]
Ophthalmic surgeons should take precautions in eyes with a history of herpes simplex keratitis (HSK) and herpes zoster ophthalmicus (HZO), said Marc Labetoulle MD, Bicêtre Hospital, Paris France.
Example of geographic keratitis observed four days after cataract surgery in a patient without previous history of herpes simplex ocular disease[/caption]
Ophthalmic surgeons should take precautions in eyes with a history of herpes simplex keratitis (HSK) and herpes zoster ophthalmicus (HZO), said Marc Labetoulle MD, Bicêtre Hospital, Paris France.
 Marc Labetoulle MD
Marc Labetoulle MDTags: herpes, herpetic disease, keratitis
Latest Articles
ESCRS Today 2025: Happy Anniversaries!
ESCRS celebrates milestones with pioneers in IOLs, LASIK, femtosecond lasers, and corneal transplantation.
ESCRS Today 2025: A Congress for Everyone
From YOs to families, the ESCRS Annual Meeting embraces full participation through inclusivity.
Beyond the Numbers
Empowering patient participation fosters continuous innovation in cataract surgery.
Thinking Beyond the Surgery Room
Practice management workshop focuses on financial operations and AI business applications.
Aid Cuts Threaten Global Eye Care Progress
USAID closure leads retreat in development assistance.
Supplement: ESCRS Clinical Trends Series: Presbyopia
Debate: FS-LASIK or KLEx for Hyperopia?
FS-LASIK has more of a track record, but KLEx offers advantages.
Four AI Applications Ready for Practice
Commercial offerings may save time, improve practice and research.
Perioperative Medication Regimens for Cataract Surgery
Randomised controlled clinical trial results provide evidence-based guidance.