Presbyopic Lens Exchange
Communication crucial to maximising outcomes in presbyopes. Roibeárd O’hÉineacháin reports.

Roibeard O’hEineachain
Published: Tuesday, May 31, 2022
The key to ensuring satisfaction in refractive lens exchange patients is achieving a visual postoperative vision that suits their visual and lifestyle requirements better than what they had with their natural crystalline lens, emphasises Francesco Carones MD.
“Visual acuity improvement is not the only goal anymore. Europeans aged 55 years or older spend at least six hours a day on leisure and sports activities as well as other daily activities and occupational needs that involve several working distances,” he said.
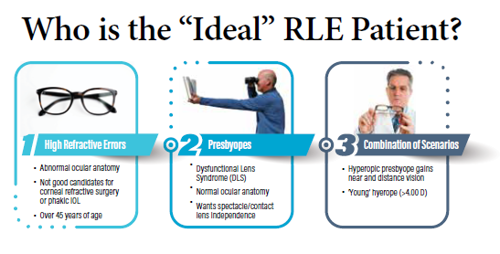
Dr Carones noted several major differences between patients who seek clear lens exchange for high ametropia and those who wish to undergo refractive lens exchange for presbyopia. In high ametropes, clear lens exchange aims to reduce the degree of correction needed with spectacles or contact lenses. Such patients seldom receive presbyopia-correcting IOLs, and emmetropia without correction is not always the goal.
Patients seeking presbyopia correction from lens exchange include those with cataracts and those seeking treatment for presbyopia. Both groups have a strong desire for spectacle independence. However, as with high ametropes, the lens exchange aspect of the procedure in cataract patients is therapeutic, and an uneventful surgery with some degree of spectacle independence may satisfy their principal motivation, Dr Carones said.
In contrast, spectacle independence is the principal motivation for refractive lens exchange in presbyopes without cataracts, and such patients may be more disappointed with their outcomes if they need spectacle correction for daily activities. As it is an elective procedure, presbyopia patients may be more sensitive to any loss in uncorrected distance visual acuity.
Moreover, presbyopes need to understand refractive lens exchange procedures carry the same risks as cataract surgery, such as posterior capsule opacification, cystoid macular oedema (CME), and endophthalmitis. Furthermore, myopes undergoing such procedures are at an increased risk of retinal detachment.
When counselling presbyopia patients considering refractive lens exchange, Dr Carones noted the importance of explaining dysfunctional lens syndrome (DLS), differentiating the inflexible presbyopic lens from the early stages of cataract. Using advanced diagnostics and a proper DLS grading scale can educate patients on their condition and help determine the best procedure in their case.
In addition, he advised listening to the patient as they express their needs and concerns regarding their vision. At the same time, the clinician must take the role of the expert, making confident recommendations, using straightforward, consistent language, and explaining the rationale behind their recommendations.
It is also important to consider factors that may affect postoperative visual outcomes and patient satisfaction. When considering which IOL to use, the physician needs to determine what kinds of compromise the patient is willing to accept – such as the need for spectacle correction for reading or the presence of halos in scotopic conditions—emphasising to the patient there is no perfect lens design.
“Messaging is crucial. Therefore, educate patients on important diagnostic information and show them why they are or are not good candidates. Refractive lens exchange is an elective procedure, so you need to ensure postoperative vision quality and refractive outcomes are comparable, if not better, than what they have with the crystalline lens,” Dr Carones concluded.
This presentation was made at the ESCRS Virtual Winter Meeting 2022.
Francesco Carones MD is the Medical Director and Physician CEO at Carones Vision Advalia, Milan, Italy.
Latest Articles
Beyond the Numbers
Empowering patient participation fosters continuous innovation in cataract surgery.
Thinking Beyond the Surgery Room
Practice management workshop focuses on financial operations and AI business applications.
Picture This: Photo Contest Winners
ESCRS 2025 Refractive and Cataract Photo Contest winners.
Aid Cuts Threaten Global Eye Care Progress
USAID closure leads retreat in development assistance.
Supplement: ESCRS Clinical Trends Series: Presbyopia
Nutrition and the Eye: A Recipe for Success
A look at the evidence for tasty ways of lowering risks and improving ocular health.
New Award to Encourage Research into Sustainable Practices
Sharing a Vision for the Future
ESCRS leaders update Trieste conference on ESCRS initiatives.
Extending Depth of Satisfaction
The ESCRS Eye Journal Club discuss a new study reviewing the causes and management of dissatisfaction after implantation of an EDOF IOL.
Conventional Versus Laser-Assisted Cataract Surgery
Evidence favours conventional technique in most cases.