Myopic foveoschisis
Early intervention correlates with better functional outcome

Cheryl Guttman Krader
Published: Friday, March 1, 2019
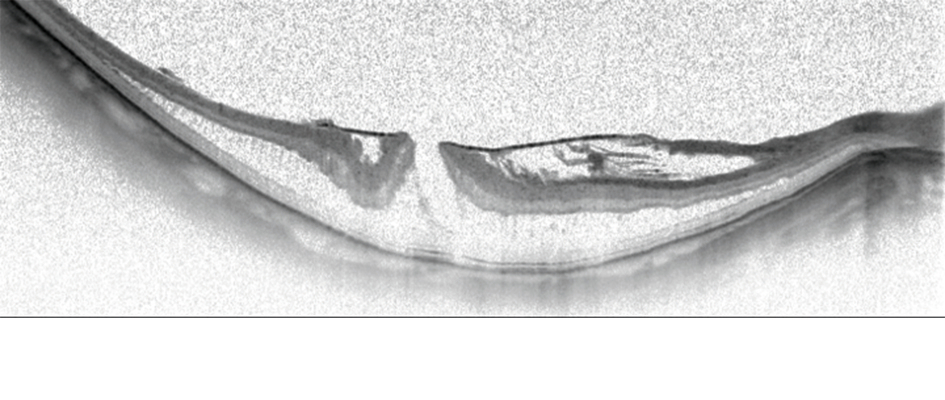 Horizontal OCT scan of a myopic foveoschisis with a premacular membrane[/caption]
Preoperative visual acuity is the main factor influencing functional outcomes after vitrectomy for myopic foveoschisis. With this information in mind, retina specialists aiming to improve their results should consider operating sooner rather than later, said Ramin Tadayoni MD, PhD, at the 18th EURETINA Congress in Vienna, Austria.
“Of course, we can also do better for our patients by using modern surgical techniques and imaging technologies. But, we will have better results if the indication for surgery is good. If the goal is to achieve BCVA [best-corrected visual acuity] better than 20/40, then surgery should be done when the vision is 20/50 or better. We should not wait for the vision to get worse,” said Dr Tadayoni, Professor of Ophthalmology, Paris 7 University, Lariboisière Hospital & OphtalmoPôle, Paris, France.
Horizontal OCT scan of a myopic foveoschisis with a premacular membrane[/caption]
Preoperative visual acuity is the main factor influencing functional outcomes after vitrectomy for myopic foveoschisis. With this information in mind, retina specialists aiming to improve their results should consider operating sooner rather than later, said Ramin Tadayoni MD, PhD, at the 18th EURETINA Congress in Vienna, Austria.
“Of course, we can also do better for our patients by using modern surgical techniques and imaging technologies. But, we will have better results if the indication for surgery is good. If the goal is to achieve BCVA [best-corrected visual acuity] better than 20/40, then surgery should be done when the vision is 20/50 or better. We should not wait for the vision to get worse,” said Dr Tadayoni, Professor of Ophthalmology, Paris 7 University, Lariboisière Hospital & OphtalmoPôle, Paris, France.
 Ramin Tadayoni MD, PhD
Ramin Tadayoni MD, PhDTags: myopic foveoschisis, vitrectomy
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.