Cornea
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.

Soosan Jacob
Published: Tuesday, July 1, 2025
Optical quality of the eye is affected not just by higher-order aberrations (HOAs) but also by diffraction and scatter. Thus, even the perfect lens has a limit to its resolution.
Diffraction
Fraunhofer diffraction occurs when light passes through a circular aperture, known as an Airy disc. The Airy disc or pattern refers to the best possible focused spot of light created by the diffraction pattern formed when light passes through a perfect lens with a circular aperture. A uniformly illuminated circular aperture creates a bright central spot, followed by a series of concentric rings. An optical system where the resolution is not limited by any HOAs but only by diffraction is called a diffraction-limited optical system. Except with a very small pupil, even the best eyes have optical quality below the diffraction limit.
Scatter
Ocular scatter can degrade the visual image just as HOAs and diffraction can. This occurs due to light passing through media with optical inhomogeneity—i.e., spatial variations in the refractive index. Scatter is due to a combination of refraction, reflection, and diffraction. For example, scatter can occur secondary to a synthetic intracorneal ring segment within the cornea of a different refractive index. Incident light would get partly reflected, partly refracted, and partly undergo internal reflections before getting refracted/reflected again. Light falling at the edge would also undergo diffraction. These phenomena cause retinal image degradation, resulting in glare and hazy vision. Scatter causes local disturbances to the wavefront but are not responsible for shape errors.
Higher-order aberrations
Discussed in part one of this series (May/June 2025 issue), HOAs are basically responsible for an irregular wavefront as opposed to a plane (parallel rays) or spherical (converging or diverging rays that come to a point focus) wavefront. HOAs are primarily due to corneal pathology, although other conditions such as crystalline lens or the IOL may also be responsible. Total ocular aberrations are composed of corneal aberrations and internal aberrations.
Wave aberration and aberrometry
This quantifies the overall magnitude of wavefront deviations from an ideal wavefront. It is plotted in microns on the exit pupil and dependent on pupil size. Aberrometry refers to measurement of the HOAs. Aberrometers are used to measure the ocular monochromatic HOAs. The result is shown as an aberration map describing the variation in the optical path distance from the source to the retinal image through each point of the pupil. It is important to look at not only the magnitude of each mode but also the possible combinations, as certain combinations can change overall retinal image quality and, therefore, visual acuity. Many devices can measure ocular aberrations:
Hartmann-Shack aberrometer A narrow laser beam is focused on the retina to generate a point source. The outcoming light rays experiencing all the ocular aberrations are split into multiple focal spots by a lenslet array on a CCD camera, with their displacement from the ideal used to reconstruct the wavefront. This is less effective for highly irregular corneas such as keratoconus and post-surgical corneas. Examples include the Zywave aberrometer (Bausch + Lomb) and VISX WaveScan (AMO).
Tscherning aberrometer A grid of laser spots is projected onto the retina, and a camera captures the distorted pattern to determine wavefront errors. This can work better in cases with highly irregular corneas but is less commonly used. The WaveLight Allegro Analyzer (Allegro) is one example.
Raytracing aberrometer A thin laser beam is directed into the eye parallel to the visual axis. Each entrance point provides a projection on the retina, which is measured. A set of entrance points forms a set of projections, and a refraction map is reconstructed from these data. It works well in highly aberrated eyes. The iTrace (Tracey Technologies) is an example.
Dynamic skiascopy Dynamic skiascopy is based on principles of time-based clinical retinoscopy. A projecting apparatus shines a scanning slit of light through a projecting lens and a set of mirrors. This light reflected off the retina passes through another lens (a receiving lens) and an aperture, ending on a set of photodetectors. Both the projecting and receiving systems rotate synchronously, allowing a comparison between the perceived light and the initially projected slit-shaped beams of light. The OPD-Scan aberrometer (Nidek) is an example.
Anterior and posterior corneal surface mapping The anterior and posterior corneal surfaces can be mapped by different machines, and Zernike polynomials can be calculated from this data. Examples include the Placido disc for anterior corneal surface, OCT for posterior corneal surface in the MS-39 (CSO), and Scheimpflug imaging for both corneal surfaces in the Pentacam (Oculus).
Zernike modes
The wavefront error (WE) can be decomposed as a sum of weighted Zernike modes. The root mean square (RMS) allows quantification. Once measured, a series of polynomials is used to describe the wavefront. Each polynomial describes a mathematical wavefront shape, and the coefficient of each polynomial gives the weight of that aberration in the total wavefront map. The RMS of a perfect optical system is 0.00 microns. Mean RMS is 0.10 microns at 30 years and 0.25 microns at 60 years. The Zernike pyramid has many modes. Let us consider some of these:
Piston (Z00 ) Not a true optical aberration, as it does not model curvature in the wavefront and does not affect image quality. It causes a full shift of the image.
Tip/tilt Also not a true optical aberration, as it neither models curvature in the wavefront nor affects image quality. Horizontal tilt (Z1-1) shifts the image vertically while vertical tilt (Z11) shifts the image horizontally. Tilting the wavefront in one or two principal meridia causes a slant in the image.
Defocus, astigmatism These are the second-order aberrations that constitute the lower-order aberrations (LOAs), corrected with spherocylindrical glasses.
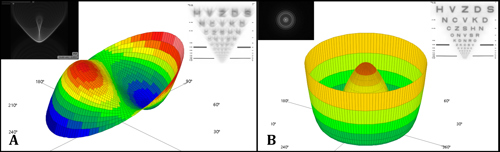
Coma Coma is a third-order aberration and causes a comet-shaped pattern, i.e., a point of light with a ‘tail’ (see figure). It has an area of myopia adjacent to an area of hyperopia in the same meridian. Vertical (Z3-1) and horizontal (Z31) coma are denoted in the Zernike pyramid. The optical asymmetry causes some rays to focus incorrectly, creating coma. When peripheral rays focus earlier than paraxial rays, a smaller image (lower magnification) is produced, referred to as negative coma. If peripheral rays are focused further than paraxial rays along the optical axis, they produce a larger image (greater magnification), and the aberration is termed positive coma.
Images of points far away from the optical axis are not sharp but comet-shaped since the images created are of increasing ring size. Each ring is the image generated from a specific area of the cornea, thus forming a comet shape. The ‘comet’ may have its ‘tail’ pointing away from or towards the optical axis, depending on whether the coma aberration is positive or negative, respectively, assuming there is no defocus in the system. Coma interacts with the presence of other LOA and HOA, meaning its effects become more complex and may not exactly follow the positive/negative classification.
In keratoconus, light from the retina exits the eye faster from the superior cornea and is delayed leaving the inferior cornea. This gap is magnified further because light exiting superior cornea starts travelling even faster as air has lower refractive index, which creates vertical coma aberration.
Trefoil Trefoil is another third-order aberration. It is a triangular astigmatism with three axes. Orientation varies between 30 and 150 degrees, and the values are repeated twice more every 120 degrees. Vertical trefoil (Z3-3, 90-210-330 degrees) is more frequent than horizontal (Z33, 30-150-270 degrees). Normal value ranges between 0.00 and 0.50 microns at a mean pupil diameter of 6.5 mm (< 0.25 is associated with better vision).
Trefoil has a lesser effect on image quality compared to an equal amount of coma. In most people, vertical trefoil is coupled with vertical coma, resulting in a better image quality than the trefoil or coma independently. People with large amounts of aberrations (RMS > 0.4) sometimes have coma-trefoil vertical coupling, which helps keep their acuity at good levels. In aberrated eyes, the interaction depends on the phase of the HOA, and improvement/degradation can occur. Trefoil can cause glare and halos.
Spherical aberration (Z40) Positive and negative spherical aberration—it can cause a decrease in contrast sensitivity and halos around light. Negative spherical aberration has been used to increase depth of focus. Spherical aberration will be discussed in detail in the next part of this series.
Secondary astigmatism It can have an oblique (Z4-2, 45 degrees/135 degrees) or horizontal/vertical (Z42, 0 degrees/90 degrees, WTR/ATR) orientation, is a complex, non-symmetrical wavefront distortion, and has a four-lobed pattern that cannot be fully corrected with regular cylinder.
Quadrafoil Oblique (Z4-4) at a 45/135-degree orientation and horizontal/vertical (Z44) at a 0/90-degree orientation.
Secondary coma [Vertical (Z5-1) and horizontal (Z51)]; Secondary trefoil (Z5-3 and Z53) and Pentafoil (Z5-5 and Z55) These are complex patterns that constitute fifth-order aberrations.
Aberropia
Just as myopia, hyperopia, and astigmatism refer to certain types of refractive errors, a decrease in the visual quality or quantity secondary to higher-order aberrations also needs to have a well-defined nomenclature. The often-used blanket term, irregular astigmatism, is a misnomer—for example, when considering the central column of the Zernike pyramid with rotationally symmetrical modes. We therefore coined the term aberropia in 2002 to denote refractive errors secondary to HOA. Aberropia results in a large circle of blur, increased point spread function, and decreased quality of vision. It can be congenital or acquired and can arise from the tear film (uneven tear film), cornea (keratoconus, post-LASIK ectasia, post-keratoplasty, corneal scars), lens (incipient cataract, subluxation, lenticonus, capsular striae), IOL (subluxated or decentred IOL, multifocal/extended depth of focus IOLs, other newer aberration-based IOLs), vitreous (vitreous floaters, opacities), or even retina (thickened hyaloid, fine epiretinal membrane).
This is the second in a multipart tutorial on higher-order aberrations.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.