Late LASIK flap study
No need to flap over late LASIK enhancements.

Dermot McGrath
Published: Tuesday, September 1, 2020
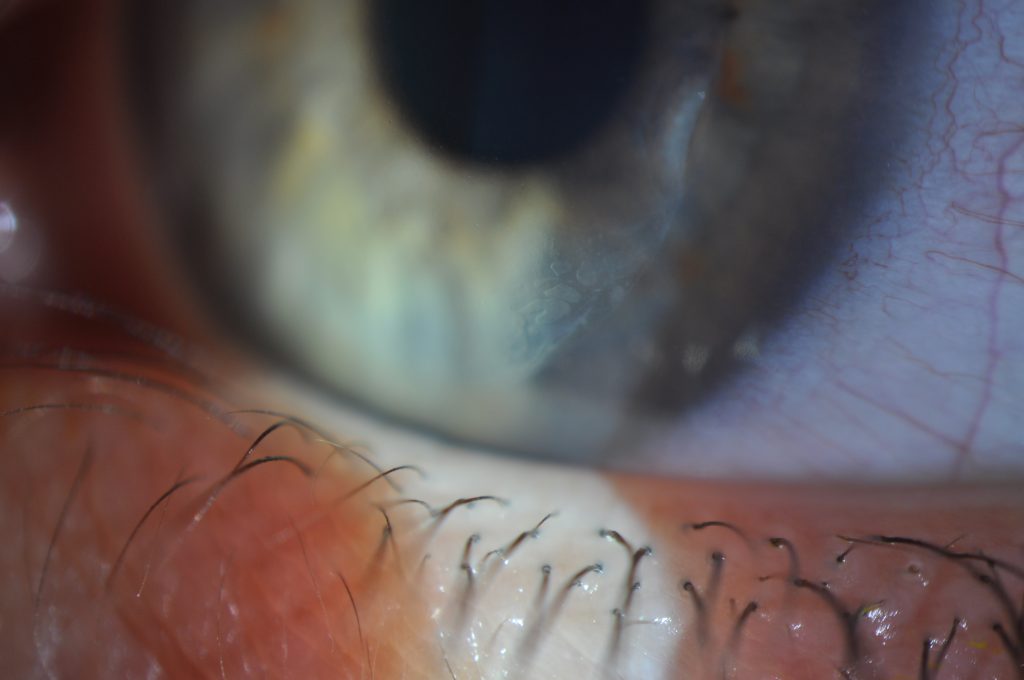 Moderate and progressive grade II epithelial ingrowth that requires treatment with YAG laser to solve the problem and avoid further progression. No need for surgical intervention if YAG laser is used for such cases[/caption]
Lifting a LASIK flap for refractive enhancement five or 10 years after the initial procedure can be safely and successfully achieved, according to Jorge Alió del Barrio MD, PhD, FEBOS-CR.
“Our study showed that flap lift for refractive enhancement up to 10 years or more after LASIK is a feasible surgical alternative, which provides good efficacy and safety with fast visual recovery. The rate of surgical intervention for significant postoperative epithelial ingrowth (EI) was low as far as early EI is properly managed with YAG laser as previously described by our group,” Dr Alió del Barrio told delegates attending the 37th Congress of the ESCRS in Paris.
Late residual refractive errors, years after the initial LASIK procedure, are a common problem faced by refractive surgeons, noted Dr Alió del Barrio, a surgeon at the Cornea, Cataract and Refractive Surgery Unit, Vissum Corporación, Alicante, Spain.
“Studies have shown that there is about a 10-year re-treatment rate of 20.8% for myopia up to -10D, and after hyperopic LASIK, a progressive increase in hyperopia from the original LASIK has also been reported up to 16 years postoperatively,” he said.
The two main options to treat refractive errors in these patients are either PRK over the flap, or a flap re-lift followed by refractive enhancement.The advantages of a late LASIK flap lift include fast visual recovery, no postoperative pain and no risk of haze, said Dr Alió del Barrio. The disadvantages of this approach are similar to the original LASIK procedure that are primarily flap related – folds, interface debris and the most important one is the risk of EI at the flap interface.
“It has been shown that the risk of epithelial ingrowth increases over time from the primary LASIK procedure, which helps to explain why the currently available literature discourages refractive surgeons from lifting LASIK flaps older than three years,” he said.
Dr Alió del Barrio’s study included 70 eyes of 48 patients. The primary LASIK procedure was myopic in 45 eyes, hyperopic in 22 eyes and presbyopic in three eyes. The flap was dissected using a mechanical microkeratome in 62 eyes (89%) and a femtosecond laser in the remaining eight eyes (11%).
The mean time from primary LASIK to the flap lift was 12.3 years. In 57 eyes, the primary LASIK flap was created at least 10 years before the enhancement. The mean pre-lift spherical equivalent was −1.29D in the myopia group and +0.65D in the hyperopia group.
Three months after the surgery, 88% of myopic eyes and 74% of hyperopic eyes had an uncorrected distance visual acuity of 20/20 or better and all patients achieved at least 20/25. No eye lost two lines or more of corrected distance visual acuity.
Mild EI developed in 31% of eyes (not requiring any intervention) and clinically significant EI in 11% of eyes, with only 4% of eyes requiring a re-lift for severe EI. As far as progressive or moderate EI is early diagnosed and treated with YAG laser, the risk for severe EI requiring a new flap lift for interface cleaning is marginal.
“Clinically relevant epithelial ingrowth is not an exceptional complication after late flap re-lift. However, an adequate noninvasive management with YAG laser minimises the risk of requiring surgical re-intervention, being an acceptable risk for both the surgeon and the patient,” he said.
Jorge Alió del Barrio: Jorge_alio@hotmail.com
Moderate and progressive grade II epithelial ingrowth that requires treatment with YAG laser to solve the problem and avoid further progression. No need for surgical intervention if YAG laser is used for such cases[/caption]
Lifting a LASIK flap for refractive enhancement five or 10 years after the initial procedure can be safely and successfully achieved, according to Jorge Alió del Barrio MD, PhD, FEBOS-CR.
“Our study showed that flap lift for refractive enhancement up to 10 years or more after LASIK is a feasible surgical alternative, which provides good efficacy and safety with fast visual recovery. The rate of surgical intervention for significant postoperative epithelial ingrowth (EI) was low as far as early EI is properly managed with YAG laser as previously described by our group,” Dr Alió del Barrio told delegates attending the 37th Congress of the ESCRS in Paris.
Late residual refractive errors, years after the initial LASIK procedure, are a common problem faced by refractive surgeons, noted Dr Alió del Barrio, a surgeon at the Cornea, Cataract and Refractive Surgery Unit, Vissum Corporación, Alicante, Spain.
“Studies have shown that there is about a 10-year re-treatment rate of 20.8% for myopia up to -10D, and after hyperopic LASIK, a progressive increase in hyperopia from the original LASIK has also been reported up to 16 years postoperatively,” he said.
The two main options to treat refractive errors in these patients are either PRK over the flap, or a flap re-lift followed by refractive enhancement.The advantages of a late LASIK flap lift include fast visual recovery, no postoperative pain and no risk of haze, said Dr Alió del Barrio. The disadvantages of this approach are similar to the original LASIK procedure that are primarily flap related – folds, interface debris and the most important one is the risk of EI at the flap interface.
“It has been shown that the risk of epithelial ingrowth increases over time from the primary LASIK procedure, which helps to explain why the currently available literature discourages refractive surgeons from lifting LASIK flaps older than three years,” he said.
Dr Alió del Barrio’s study included 70 eyes of 48 patients. The primary LASIK procedure was myopic in 45 eyes, hyperopic in 22 eyes and presbyopic in three eyes. The flap was dissected using a mechanical microkeratome in 62 eyes (89%) and a femtosecond laser in the remaining eight eyes (11%).
The mean time from primary LASIK to the flap lift was 12.3 years. In 57 eyes, the primary LASIK flap was created at least 10 years before the enhancement. The mean pre-lift spherical equivalent was −1.29D in the myopia group and +0.65D in the hyperopia group.
Three months after the surgery, 88% of myopic eyes and 74% of hyperopic eyes had an uncorrected distance visual acuity of 20/20 or better and all patients achieved at least 20/25. No eye lost two lines or more of corrected distance visual acuity.
Mild EI developed in 31% of eyes (not requiring any intervention) and clinically significant EI in 11% of eyes, with only 4% of eyes requiring a re-lift for severe EI. As far as progressive or moderate EI is early diagnosed and treated with YAG laser, the risk for severe EI requiring a new flap lift for interface cleaning is marginal.
“Clinically relevant epithelial ingrowth is not an exceptional complication after late flap re-lift. However, an adequate noninvasive management with YAG laser minimises the risk of requiring surgical re-intervention, being an acceptable risk for both the surgeon and the patient,” he said.
Jorge Alió del Barrio: Jorge_alio@hotmail.com
Tags: epithelial ingrowth, LASIK, lasik flap, refractive enhancement
Latest Articles
Nutrition and the Eye: A Recipe for Success
A look at the evidence for tasty ways of lowering risks and improving ocular health.
New Award to Encourage Research into Sustainable Practices
Sharing a Vision for the Future
ESCRS leaders update Trieste conference on ESCRS initiatives.
Extending Depth of Satisfaction
The ESCRS Eye Journal Club discuss a new study reviewing the causes and management of dissatisfaction after implantation of an EDOF IOL.
Conventional Versus Laser-Assisted Cataract Surgery
Evidence favours conventional technique in most cases.
AI Scribing and Telephone Management
Automating note-taking and call centres could boost practice efficiency.
AI Analysis and the Cornea
A combination of better imaging and AI deep learning could significantly improve corneal imaging and diagnosis.
Cooking a Feast for the Eyes
A cookbook to promote ocular health through thoughtful and traditional cuisine.
Need to Know: Spherical Aberration
Part three of this series examines spherical aberration and its influence on higher-order aberrations.
Generating AI’s Potential
How generative AI impacts medicine, society, and the environment.