Glaucoma meets AI
Researchers are employing deep learning to tackle the challenges of glaucoma diagnosis

Cheryl Guttman Krader
Published: Tuesday, July 9, 2019
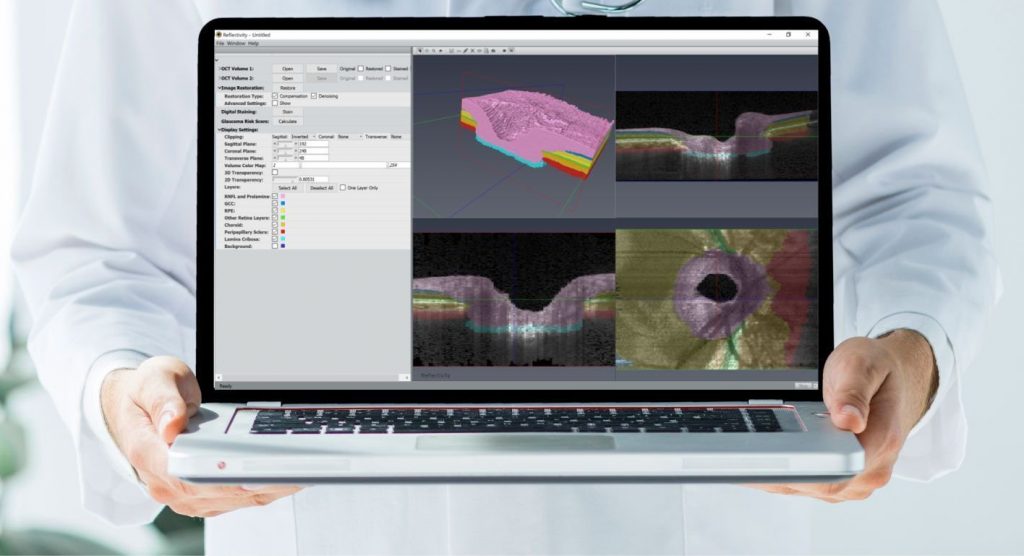 Reflectivity 4.0: a 3D AI companion to simplify and improve glaucoma management[/caption]
Image courtesy of Alexandre Thiéry PhD
Researchers at the National University of Singapore are aiming to apply deep learning to optical coherence tomography (OCT) images in order to modernise and simplify the diagnosis of glaucoma and to obtain a better understanding of how the disease progresses over time.
At the annual meeting of the Association for Research in Vision and Ophthalmology (ARVO) in Vancouver, Canada, Alexandre Thiéry PhD discussed the work being done by the Optical Coherence Tomography & Artificial Intelligence for Glaucomatous Optic Neuropathy (OCTAGON) team.
Dr Thiéry is Professor, Department of Statistics and Applied Probability, National University of Singapore, and is co-principal investigator of OCTAGON with Michaël JA Girard PhD, Professor of Biomedical Engineering, National University of Singapore, Singapore. Dr Thiéry explained that the project focuses on the optic nerve head because it represents the main site of glaucoma damage, and it is based on three-dimensional (3D) segmentation.
“Glaucoma is a complex disease that affects connective and neural tissues with 3D structural changes. By exploring these 3D structures, we can provide a diagnosis and prognosis of glaucoma more accurately than current gold standards,” Dr Thiéry said.
Dr Girard told EuroTimes: “In fact, we have empirically proven that our method is 30% more accurate at diagnosing glaucoma than traditional methods based on fundus imaging or retinal nerve fiber layer thickness assessment.”
Reflectivity 4.0: a 3D AI companion to simplify and improve glaucoma management[/caption]
Image courtesy of Alexandre Thiéry PhD
Researchers at the National University of Singapore are aiming to apply deep learning to optical coherence tomography (OCT) images in order to modernise and simplify the diagnosis of glaucoma and to obtain a better understanding of how the disease progresses over time.
At the annual meeting of the Association for Research in Vision and Ophthalmology (ARVO) in Vancouver, Canada, Alexandre Thiéry PhD discussed the work being done by the Optical Coherence Tomography & Artificial Intelligence for Glaucomatous Optic Neuropathy (OCTAGON) team.
Dr Thiéry is Professor, Department of Statistics and Applied Probability, National University of Singapore, and is co-principal investigator of OCTAGON with Michaël JA Girard PhD, Professor of Biomedical Engineering, National University of Singapore, Singapore. Dr Thiéry explained that the project focuses on the optic nerve head because it represents the main site of glaucoma damage, and it is based on three-dimensional (3D) segmentation.
“Glaucoma is a complex disease that affects connective and neural tissues with 3D structural changes. By exploring these 3D structures, we can provide a diagnosis and prognosis of glaucoma more accurately than current gold standards,” Dr Thiéry said.
Dr Girard told EuroTimes: “In fact, we have empirically proven that our method is 30% more accurate at diagnosing glaucoma than traditional methods based on fundus imaging or retinal nerve fiber layer thickness assessment.”
 Alexandre Thiéry PhD and Michaël JA Girard PhD
Alexandre Thiéry PhD and Michaël JA Girard PhDTags: optical coherence tomography, Optical Coherence Tomography and Artificial Intelligence for Glaucomatous Optic Neuropathy (OCTAGON)
Latest Articles
Addressing Postoperative Visual Complications
Managing aberrations after laser refractive surgery requires a multi-layered approach.
3D Printing Helps Transform Ukrainian Eye Care
The country’s ophthalmologists offer valuable experience in treating ocular trauma and prosthesis design.
Winning Essay Says ‘Collective Desire’ Must Drive DEI Implementation
Emerging Microbial Trends That Could Affect Your Practices
A triptych of challenges paints a concerning picture for ophthalmologists across the globe.
Improving Outcomes with Laser-Assisted Surgery
Femtosecond laser offers a multifunctional tool for improving the safety and efficacy of cataract and refractive lens exchange procedures.
Could the Corneal Transplant Pool Increase?
Modifying or discarding major contraindications for keratoplasty could mean more patients have their sight restored.
Matching Premium IOLs to Visual Lifestyles
From monofocal to full-range solutions, each practice needs comprehensive understanding.
Going Dutch on Acanthamoeba Keratitis
A world-first trial suggests a new medication could beat the disease.
Avoiding Intracorneal Ring Segment Complications
Femtosecond lasers are helping improve refractive results with fewer problems.