Ophthalmology after the COVID-19 pandemic
Paramedical training and telemedicine can help in a post-COVID era

Dermot McGrath
Published: Friday, February 19, 2021
 MAINTAINING the highest standards of ophthalmic care in the face of ever-tighter budgets and increased patient numbers against the backdrop of the COVID-19 pandemic provided the timely focus of the symposium “Too Many Patients, Too Few Doctors, Better Eyecare”, held on the opening day of the 25th ESCRS Winter Meeting Virtual 2021.
“With ageing populations and increasing demands on doctors with reduced budgets, these issues are very relevant and need to be addressed by every healthcare practitioner sooner rather than later,” remarked Prof. David Spalton, who co-chaired the symposium with Prof. Jorge Alió, assisted by a panel of experts: Drs Jacek Szaflik, Christina Nikolova Grupcheva, Cédric Schweitzer, Florian Kretz and Guy Sallet.
Opening the symposium, Nicholas Strouthidis, Medical Director of Moorfields Eye Hospital in London, UK, focused on the possibilities of training paramedical support staff to meet the challenges of delivering safe and effective eyecare.
He cited the example of Moorfields paramedical intravitreal injection programme, which has seen a dedicated team of nurses delivering injections for AMD patients and laser capsulotomies with no compromise on patient safety.
Other examples of expanded roles for paramedical staff at Moorfields include optometry-led glaucoma clinics and management of early keratoconus as well as nurse practitioners triaging, treating and discharging patients attending the eye casualty department.
“Upskilling paramedical staff to deliver low-risk, repeatable care according to strict protocols has been shown to be safe, effective and economical,” he said.
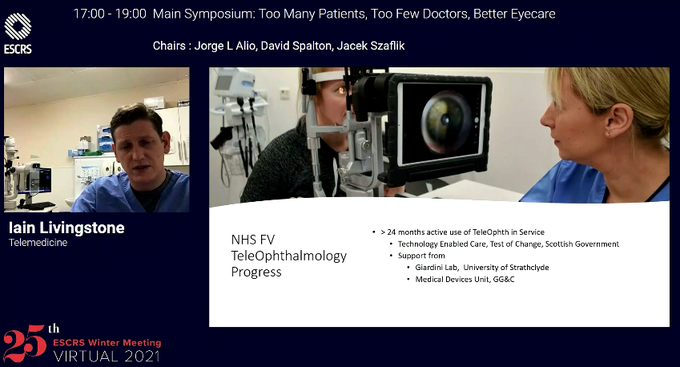
In the next presentation, Iain Livingstone MD highlighted the immense potential of telemedicine to serve dispersed populations in rural areas, reduce crowded clinics and avoid unnecessary hospital visits for patients.
Dr Livingstone discussed his experience setting up a pioneering virtual emergency teleophthalmology programme covering a large part of Scotland in response to the COVID-19 emergency. The network uses inexpensive equipment and a live video feed to securely connect doctors, opticians and patients and ensure that patients with serious eye problems can be immediately diagnosed and treated.
Rounding off the symposium, Prof. dr. Rudy MMA Nuijts presented data from a multi-centre randomised study of 865 patients at 10 hospitals in the Netherlands looking at the possible benefits of immediate sequential bilateral cataract surgery (ISBCS).
Among these potential theoretical benefits, Prof Nuijts cited less time between surgeries, fewer hospital visits, a faster total recovery period due to simultaneous postoperative care in both eyes and less use of homecare.
Summing up the results, Prof. Nuijts said that ISBCS showed comparable safety and effectiveness to delayed sequential bilateral cataract surgery (DSBCS). ISBCS also incurred lower costs compared to DSBCS but further analysis will be needed to properly assess its cost-effectiveness, he concluded.
“I think the take-home message from all our presentations is that if you are going to implement these changes then you really need to do it in the proper way and adhere to all the necessary protocols,” said Prof. Spalton. “You need to organise paramedical training properly, to set up telemedicine carefully and to implement ISBCS with the proper theatre controls. Our lives as surgeons are changing and these are issues that are going to be affecting us all in the next five years,” he concluded.
MAINTAINING the highest standards of ophthalmic care in the face of ever-tighter budgets and increased patient numbers against the backdrop of the COVID-19 pandemic provided the timely focus of the symposium “Too Many Patients, Too Few Doctors, Better Eyecare”, held on the opening day of the 25th ESCRS Winter Meeting Virtual 2021.
“With ageing populations and increasing demands on doctors with reduced budgets, these issues are very relevant and need to be addressed by every healthcare practitioner sooner rather than later,” remarked Prof. David Spalton, who co-chaired the symposium with Prof. Jorge Alió, assisted by a panel of experts: Drs Jacek Szaflik, Christina Nikolova Grupcheva, Cédric Schweitzer, Florian Kretz and Guy Sallet.
Opening the symposium, Nicholas Strouthidis, Medical Director of Moorfields Eye Hospital in London, UK, focused on the possibilities of training paramedical support staff to meet the challenges of delivering safe and effective eyecare.
He cited the example of Moorfields paramedical intravitreal injection programme, which has seen a dedicated team of nurses delivering injections for AMD patients and laser capsulotomies with no compromise on patient safety.
Other examples of expanded roles for paramedical staff at Moorfields include optometry-led glaucoma clinics and management of early keratoconus as well as nurse practitioners triaging, treating and discharging patients attending the eye casualty department.
“Upskilling paramedical staff to deliver low-risk, repeatable care according to strict protocols has been shown to be safe, effective and economical,” he said.
In the next presentation, Iain Livingstone MD highlighted the immense potential of telemedicine to serve dispersed populations in rural areas, reduce crowded clinics and avoid unnecessary hospital visits for patients.
Dr Livingstone discussed his experience setting up a pioneering virtual emergency teleophthalmology programme covering a large part of Scotland in response to the COVID-19 emergency. The network uses inexpensive equipment and a live video feed to securely connect doctors, opticians and patients and ensure that patients with serious eye problems can be immediately diagnosed and treated.
Rounding off the symposium, Prof. dr. Rudy MMA Nuijts presented data from a multi-centre randomised study of 865 patients at 10 hospitals in the Netherlands looking at the possible benefits of immediate sequential bilateral cataract surgery (ISBCS).
Among these potential theoretical benefits, Prof Nuijts cited less time between surgeries, fewer hospital visits, a faster total recovery period due to simultaneous postoperative care in both eyes and less use of homecare.
Summing up the results, Prof. Nuijts said that ISBCS showed comparable safety and effectiveness to delayed sequential bilateral cataract surgery (DSBCS). ISBCS also incurred lower costs compared to DSBCS but further analysis will be needed to properly assess its cost-effectiveness, he concluded.
“I think the take-home message from all our presentations is that if you are going to implement these changes then you really need to do it in the proper way and adhere to all the necessary protocols,” said Prof. Spalton. “You need to organise paramedical training properly, to set up telemedicine carefully and to implement ISBCS with the proper theatre controls. Our lives as surgeons are changing and these are issues that are going to be affecting us all in the next five years,” he concluded.
Tags: ophthalmology after covid, ESCRS Winter Virtual 2021
Latest Articles
Simulators Benefit Surgeons and Patients
Helping young surgeons build confidence and expertise.
Making Female Leadership More than a Moment
A remarkable global confluence of women in key positions.
ESCRS Talks Technology at AAO
Europe adopts technological advances, US still waiting for lenses and lasers.
Sorting Out Simultaneous Vision IOLs
The ESCRS Eye Journal Club discuss a new landmark paper on IOL classification and the need for harmonisation of terminology for presbyopic IOLs.
Big Advantages to Small-Aperture IOLs
Small-aperture IOLs offer superior image quality with increased range of focus.
Prioritising Self-Care
Benefits of maintaining physical, emotional, and mental health extend beyond the personal sphere.
Valuing Clinical Trial Design
How inclusivity and diversity can enhance scientific accuracy in research.
Knowing Iris Repair: Using Iridodiathermy in Iris Surgery
Prepare for decentred pupils and uneven irides in multiple situations.
Neuroprotectant Treatment for MacTel Type 2
Intravitreal implant releasing ciliary neurotrophic factor found safe and effective in pivotal trials.