The latest version of the Belin ABCD keratoconus progression display has been updated to include data to objectively evaluate progression after corneal cross-linking (CXL) treatment.
Speaking at the 25th ESCRS Winter Meeting, Michael W Belin MD, professor of ophthalmology and vision science at the University of Arizona, said the software enhancement should prove a valuable addition to the standard Pentacam software that incorporates the Belin ABCD progression display.
“We recently tested this new version of the software in a study carried out in Switzerland and Germany and concluded that post CXL measurement variance or ‘noise’ can be used to determine progressive change in patients after their cross-linking treatment. The noise measurements were consistent across different centres and over the course of the follow-up period,” he said.
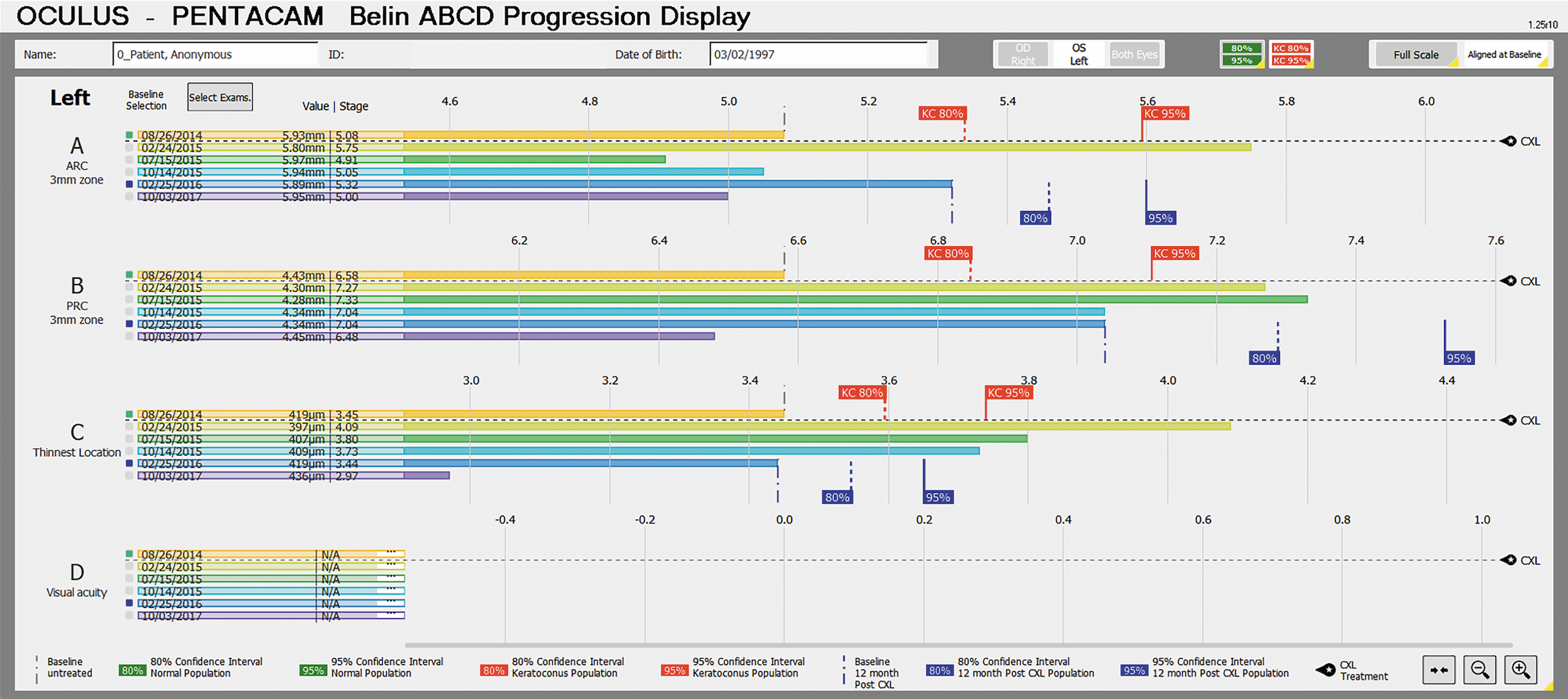
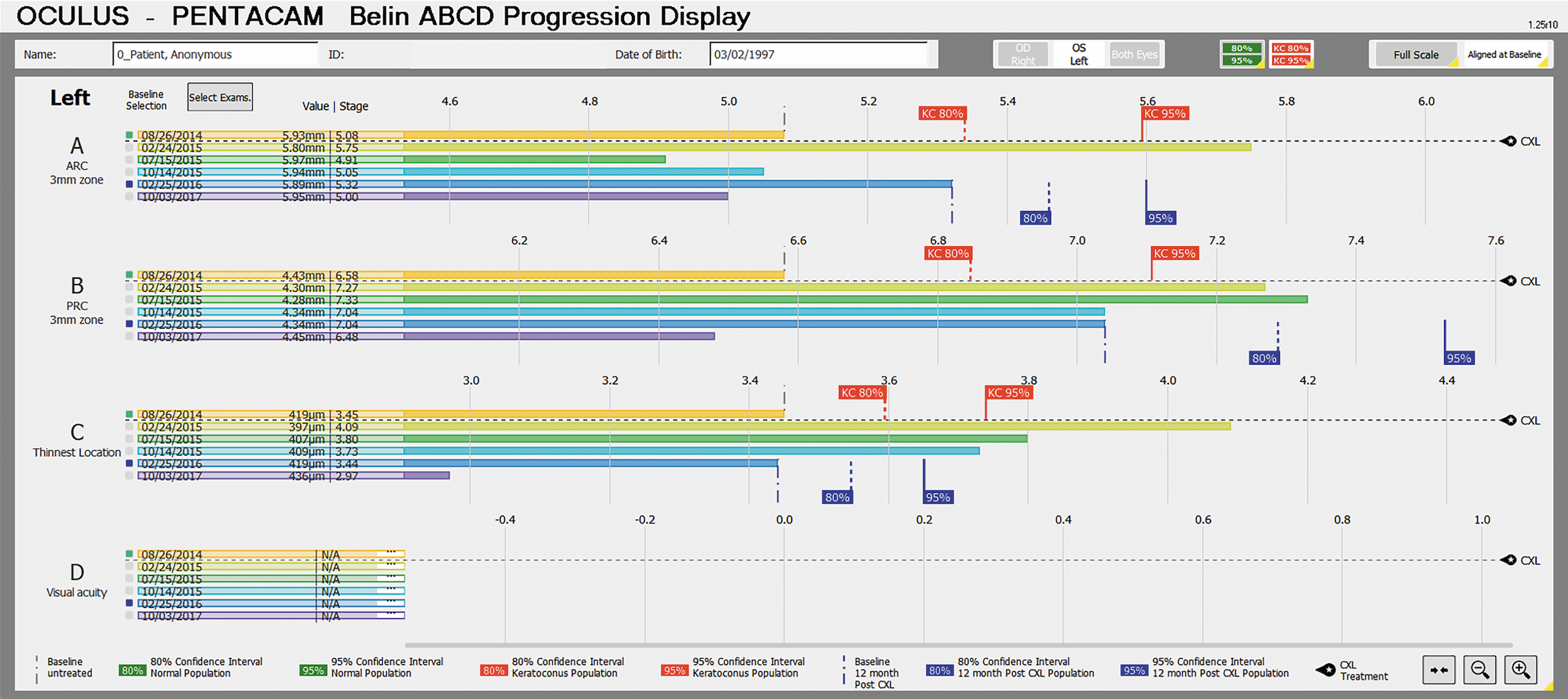
The Belin ABCD system utilises four key parameters to determine keratoconus progression: Anterior (“A”) and posterior (“B” for Back) radius of curvature taken from a 3.0 mm optical zone centred on the thinnest point, “C” is minimal Corneal thickness, and “D” best spectacle Distance visual acuity. The first three parameters (A, B, C) are machine-generated objective measurements that can be used to determine progressive change.
The ABCD Progression Display graphically displays each parameter and shows when statistical change above measurement noise is reached using colour-coded maps.
Prior to this upgrade, progression parameters after CXL were largely unknown, noted Dr Belin.
“There is not much known about post-CXL progression and the possible need for repeat treatments. All the confidence interval gates on the Belin ABCD progression display were removed once a CXL treatment was performed in earlier versions of the software,” he said.
In the study carried out in conjunction with the ELZA Institute in Zurich, Switzerland, and the Homburg Keratoconus Centre in Germany, Dr Belin and co-workers evaluated a group of 60 patients aged 11 to 66 years in a time span from 12 to 115 months after CXL treatment.
Three separate and consecutive Pentacam measurements were taken, removing the patient from the device between each measurement. A minimum of 7.5 mm of corneal coverage and an acceptable Pentacam quality score was required for inclusion. Both pooled variance and one-sided confidence intervals were then computed. The two populations had similar ABC values and similar noise measurements, noted Dr Belin.
From now on, the confidence intervals for post-CXL changes will be shown by blue gates in the Belin ABCD keratoconus progression display.
“These gates will only appear if a CXL treatment is marked and will only appear for the examinations 12 months after the treatment date to allow for epithelial healing and stromal haze to resolve,” he concluded.