Coronavirus and ophthalmology
What can ophthalmologists do to protect themselves, staff and patients from COVID-19?

Priscilla Lynch
Published: Wednesday, March 11, 2020
 The emergence of the novel coronavirus SARS-CoV-2, and the resulting disease COVID-19, in December 2019 has created a major international public health challenge.
Having spread rapidly across parts of China initially, it has subsequently spread to multiple countries across the world, with the situation ever evolving.
While COVID-19 is not as deadly as other recent new coronaviruses such as SARS and MERS, with a fatality rate of about 3.4% (as of 10 March 2020), it is far more infectious, notes Dr John Chang MD, Consultant Ophthalmologist, Hong Kong Sanitorium and Hospital. Patients can be asymptomatic for days and perhaps weeks and be transmitting the virus to others during that period.
The majority of COVID-19 cases to date, around 80%, have been mild, with those most at risk of serious disease being the elderly or people with underlying health conditions, which is important to note, Dr Chang told EuroTimes.
However, a number of healthcare workers have also died from COVID-19, including the first doctor to raise the alarm about the novel coronavirus, Dr Li Wenliang, MD, a 33-year-old ophthalmologist working in Wuhan, China, Dr Chang acknowledged.
Ophthalmologists are one of the more at-risk medical specialities for this new pathogen due to the close physical contact nature of their work, he said. Anecdotal reports suggest COVID-19 can cause conjunctivitis and possibly be transmitted by aerosol contact with conjunctiva, but this remains to be confirmed.
While official advice and protocols vary from country to country, the World Health Organization (WHO) has recommended using protection for the mouth, nose and eyes when caring for patients potentially infected with COVID-19, and self-isolation for 14 days for anyone suspected of being in contact with an infected person.
The European Centre for Disease Prevention and Control (ECDC) has also issued guidance documents on infection control and personal protective equipment (PPE) needs in healthcare settings where patients suspected/confirmed of COVID-19 infection are being treated, as well as regular updates on the spread of the disease (www.ecdc.eu).
In addition, emerging data on the disease and patient studies are being shared by the international medical community, with findings being published instantly online in journals such as The Lancet.
Speaking to EuroTimes, Dr Cillian De Gascun MD, Medical Virologist and head of Ireland’s COVID-19 Expert Advisory Group, said healthcare professionals need to ensure good infection prevention and control practices as standard, and take appropriate contact and droplet precautions, particularly for direct contact with potential COVID-19-infected patients.
“We’re still learning about this novel coronavirus and how transmissible it is; however, casual contact does not appear to constitute a significant risk. It seems to be, from the cases described in the literature, that close unprotected contact is the main risk factor for acquisition. Droplet transmission results from coughing, sneezing and contamination of the surrounding environment, including door handles and surfaces etc. as opposed to widespread community transmission,” he said, adding that there is no evidence at this point that the virus is airborne.
“So what doctors and hospitals need to do, first of all, is try to prevent contamination of surfaces, and infection of individuals so that means protecting the mucus membranes and good hand hygiene.”
Standard infection protection measures “do work and are effective” on SARS-CoV-2, and there is no evidence it is particularly resistant to existing decontamination methods, Dr De Gascun stressed.
Eye protection
“As so often is the case, ophthalmologists often lead the way and in the case of this coronavirus it is interesting that it was an ophthalmologist who picked up the disease well ahead of anyone else and sadly contracted the condition from an asymptomatic patient and later died,” Dr Sheraz Daya FRCOphth, Medical Director, Centre for Sight clinics, UK, told EuroTimes.
“We as ophthalmologists are at considerably high risk, considering we are in close proximity to patients when examining them and transmission can be through mucous membranes, including the eyes,” he said.
“I have been trying to figure out how perhaps to adapt a slit lamp and install a large protective barrier between the oculars and the examination stage. The small barrier that exists on some slit lamps is woefully inadequate.”
Dr Daya’s practice has been monitoring the international situation closely and following UK Department of Health guidance; ascertaining if patients are at risk of being infected with COVID-19 before they are seen. In countries dealing with serious outbreaks, “it makes sense for all coming into close contact [with patients] to wear eye protection and consider wearing effective face masks”, Dr Daya said.
In the meantime, Dr Chang said ophthalmologists working in private practice must also prepare for the potential financial implications of COVID-19, as in Hong Kong, procedures in his private clinic reduced drastically over the quarantine period in the region.
[caption id="attachment_18265" align="alignleft" width="1024"]
The emergence of the novel coronavirus SARS-CoV-2, and the resulting disease COVID-19, in December 2019 has created a major international public health challenge.
Having spread rapidly across parts of China initially, it has subsequently spread to multiple countries across the world, with the situation ever evolving.
While COVID-19 is not as deadly as other recent new coronaviruses such as SARS and MERS, with a fatality rate of about 3.4% (as of 10 March 2020), it is far more infectious, notes Dr John Chang MD, Consultant Ophthalmologist, Hong Kong Sanitorium and Hospital. Patients can be asymptomatic for days and perhaps weeks and be transmitting the virus to others during that period.
The majority of COVID-19 cases to date, around 80%, have been mild, with those most at risk of serious disease being the elderly or people with underlying health conditions, which is important to note, Dr Chang told EuroTimes.
However, a number of healthcare workers have also died from COVID-19, including the first doctor to raise the alarm about the novel coronavirus, Dr Li Wenliang, MD, a 33-year-old ophthalmologist working in Wuhan, China, Dr Chang acknowledged.
Ophthalmologists are one of the more at-risk medical specialities for this new pathogen due to the close physical contact nature of their work, he said. Anecdotal reports suggest COVID-19 can cause conjunctivitis and possibly be transmitted by aerosol contact with conjunctiva, but this remains to be confirmed.
While official advice and protocols vary from country to country, the World Health Organization (WHO) has recommended using protection for the mouth, nose and eyes when caring for patients potentially infected with COVID-19, and self-isolation for 14 days for anyone suspected of being in contact with an infected person.
The European Centre for Disease Prevention and Control (ECDC) has also issued guidance documents on infection control and personal protective equipment (PPE) needs in healthcare settings where patients suspected/confirmed of COVID-19 infection are being treated, as well as regular updates on the spread of the disease (www.ecdc.eu).
In addition, emerging data on the disease and patient studies are being shared by the international medical community, with findings being published instantly online in journals such as The Lancet.
Speaking to EuroTimes, Dr Cillian De Gascun MD, Medical Virologist and head of Ireland’s COVID-19 Expert Advisory Group, said healthcare professionals need to ensure good infection prevention and control practices as standard, and take appropriate contact and droplet precautions, particularly for direct contact with potential COVID-19-infected patients.
“We’re still learning about this novel coronavirus and how transmissible it is; however, casual contact does not appear to constitute a significant risk. It seems to be, from the cases described in the literature, that close unprotected contact is the main risk factor for acquisition. Droplet transmission results from coughing, sneezing and contamination of the surrounding environment, including door handles and surfaces etc. as opposed to widespread community transmission,” he said, adding that there is no evidence at this point that the virus is airborne.
“So what doctors and hospitals need to do, first of all, is try to prevent contamination of surfaces, and infection of individuals so that means protecting the mucus membranes and good hand hygiene.”
Standard infection protection measures “do work and are effective” on SARS-CoV-2, and there is no evidence it is particularly resistant to existing decontamination methods, Dr De Gascun stressed.
Eye protection
“As so often is the case, ophthalmologists often lead the way and in the case of this coronavirus it is interesting that it was an ophthalmologist who picked up the disease well ahead of anyone else and sadly contracted the condition from an asymptomatic patient and later died,” Dr Sheraz Daya FRCOphth, Medical Director, Centre for Sight clinics, UK, told EuroTimes.
“We as ophthalmologists are at considerably high risk, considering we are in close proximity to patients when examining them and transmission can be through mucous membranes, including the eyes,” he said.
“I have been trying to figure out how perhaps to adapt a slit lamp and install a large protective barrier between the oculars and the examination stage. The small barrier that exists on some slit lamps is woefully inadequate.”
Dr Daya’s practice has been monitoring the international situation closely and following UK Department of Health guidance; ascertaining if patients are at risk of being infected with COVID-19 before they are seen. In countries dealing with serious outbreaks, “it makes sense for all coming into close contact [with patients] to wear eye protection and consider wearing effective face masks”, Dr Daya said.
In the meantime, Dr Chang said ophthalmologists working in private practice must also prepare for the potential financial implications of COVID-19, as in Hong Kong, procedures in his private clinic reduced drastically over the quarantine period in the region.
[caption id="attachment_18265" align="alignleft" width="1024"]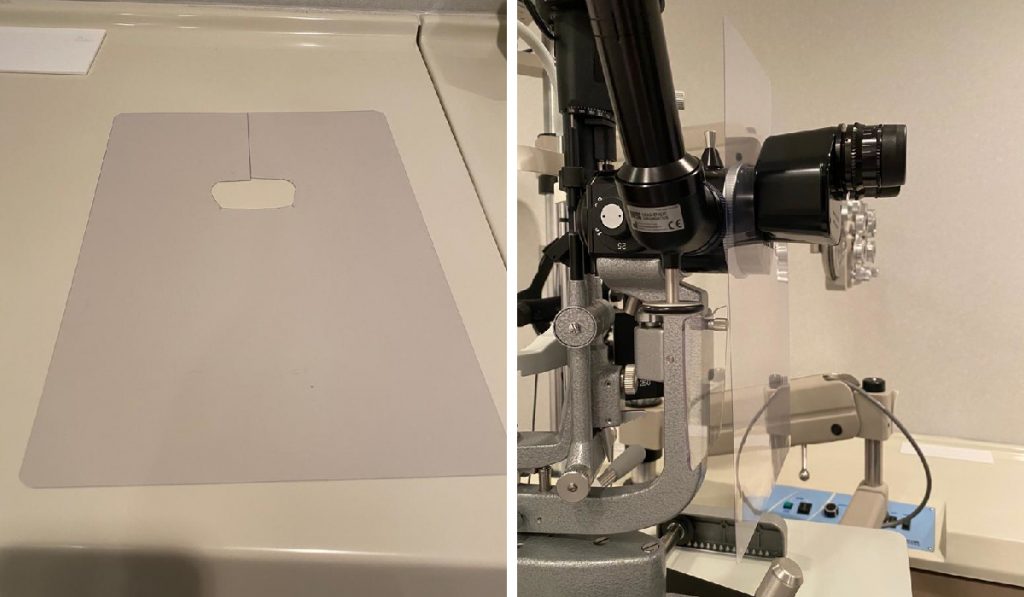 A large clear plastic sheet with a hole cut into it placed between the ocular and slit lamp. Courtesy of John SM Chang MD[/caption]
Some practical tips for the ophthalmologist from Dr Chang
The Goldman applanator (not only the tip but also the black housing) can touch the patient’s mask or mouth and transmit the virus to the examiner, so care should be taken to avoid not touching the applanator housing and sterilise it every time it is used.
A large A4-sized clear plastic sheet made for book binding covers can be purchased from any stationary store and a hole can be cut to fit between the ocular and slit lamp. One of our Hong Kong ophthalmology colleagues used his old MRI scan and mounted it on to his slit lamp!
The European Society of Cataract and Refractive Surgeons (ESCRS) is also carefully monitoring the situation through the WHO website, in relation to guidance regarding its upcoming educational meetings. See here.
Dr Cillian De Gascun: nvrldirectorsoffice@ucd.ie
Dr John Chang: John.SM.Chang@hksh.com
Dr Sheraz Daya: admin@centreforsight.com
A large clear plastic sheet with a hole cut into it placed between the ocular and slit lamp. Courtesy of John SM Chang MD[/caption]
Some practical tips for the ophthalmologist from Dr Chang
The Goldman applanator (not only the tip but also the black housing) can touch the patient’s mask or mouth and transmit the virus to the examiner, so care should be taken to avoid not touching the applanator housing and sterilise it every time it is used.
A large A4-sized clear plastic sheet made for book binding covers can be purchased from any stationary store and a hole can be cut to fit between the ocular and slit lamp. One of our Hong Kong ophthalmology colleagues used his old MRI scan and mounted it on to his slit lamp!
The European Society of Cataract and Refractive Surgeons (ESCRS) is also carefully monitoring the situation through the WHO website, in relation to guidance regarding its upcoming educational meetings. See here.
Dr Cillian De Gascun: nvrldirectorsoffice@ucd.ie
Dr John Chang: John.SM.Chang@hksh.com
Dr Sheraz Daya: admin@centreforsight.com