Cornea
Bioengineered Endothelial Implant Shows Promising in vivo Results
Scaffold-based system is easy to deploy and has short learning curve.

Sean Henahan
Published: Monday, December 1, 2025
A bioengineered, 3D printed endothelial keratoplasty implant could offer an alternative to conventional donor tissue in diseases where the corneal endothelium fails, such as Fuchs’ dystrophy and bullous keratopathy, reported Michael Mimouni MD.
“Do we even need innovations in the area of endothelial keratoplasty?” he asked. “We already have excellent techniques, including ultrathin DSAEK and DMEK. These methods have limitations, with the main one being a lack of tissue availability. According to global reports, for every 70 patients who need a corneal transplant, there is one implant available.”
Surgical approaches to addressing the tissue shortage include techniques such as DSO, quarter DMEK, and hemi-DMEK to optimise available resources. Newer technologies include artificial implants (such as EndoArt) and cell-based approaches, either scaffold-based or cell injection-based.
Dr Mimouni presented an update on a scaffold-based system called Precise-BIovision endothelial keratoplasty (PVEK). A monocellular layer of endothelial cells is printed at a density of more than 5,000 cells per square millimetre on an 8-micron-thin collagen tissue. Viability exceeds 90%.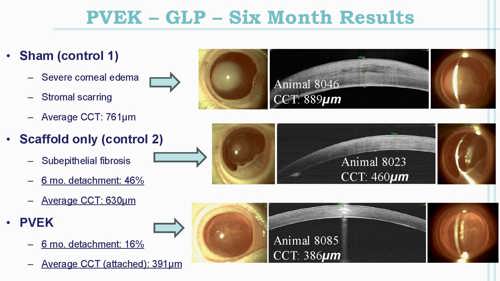
It comes pre-stamped and preloaded in a Geuder cannula. After performing descemetorhexis, the implant is inserted through a small incision, unfolded, positioned, and held in place with a gas tamponade.
“This implant is very easily deployed with minimal manipulation,” Dr Mimouni reported. “It is much easier to unfold than a DMEK and reminiscent of an ultrathin DSAEK. We are able to produce 300 tissues from one donor.”
Presenting results of in vivo research with 64 rabbits, Dr Mimouni explained one-third received the implant seeded with human corneal endothelial cells, one-third the scaffold alone, and the remainder underwent sham surgery. All underwent unilateral descemetorhexis of the right eye. Subacute (4-week) and chronic (26-week) endpoints were assessed.
“In the sham group that underwent descemetorhexis only, we found severe corneal oedema followed by stromal scarring. In the scaffold-only group, we saw that most animals developed subepithelial fibrosis and that there was a 46% detachment rate, with all those animals developing severe oedema,” he said. “The overall average central corneal thickness was 630 microns. In the PVEK group, at 6 months we saw a 16% detachment rate with a significantly lower average central corneal thickness of 391 microns.”
Some of the potential advantages of PVEK, according to Dr Mimouni, include the ability to choose the size of the implant, the shape of the marking, and the density of the endothelial cells. Moreover, the learning curve is shorter than with DMEK since the transplant is very easy to deploy.
A phase I clinical trial is in planning stages.
Dr Mimouni presented during a free paper session at the 2025 ESCRS Congress in Copenhagen.
Michael Mimouni MD serves as an attending physician and director of the Cornea Unit in the Department of Ophthalmology at Rambam Health Care Campus, Israel.