 LogMAR Visual Acuity outcomes
LogMAR Visual Acuity outcomes

Dimitrios Chiras MD, PhD, FEBO
With appropriate surgical technique, cataract surgery following vitrectomy can be safe and effective with refractive outcomes similar to those achieved in non-vitrectomised eyes, although the underlying retinal pathology may limit visual acuity and increase the risk of complications, Dimitrios Chiras MD, PhD, FEBO, Moorfields Eye Hospital, London, UK, told the 23rd ESCRS Winter Meeting in Athens Greece.
In a retrospective study, Dr Chiras and associates analysed data from consecutive patients undergoing cataract surgery between January 2015 and August 2017. Patients without postoperative visual acuity data were excluded. The study included 149 vitrectomised eyes and 608 non-vitrectomised eyes (reference group) in whom they compared best-corrected visual acuity, refractive outcomes and intraoperative and postoperative complications
The indications for pars plana vitrectomy were retinal detachment in 111 (74%) eyes, macular hole in 18 (12%) eyes, epiretinal membrane in 13 (9%) eyes, vitreomacular traction in three (2%) eyes, diabetic retinopathy in two eyes (1%), floaters in one (0.7%) eye and injury in one eye (0.7%).
Consultants performed the cataract surgery in 73% of the vitrectomised eyes and in 48% of the non-vitrectomised eyes. Fellows performed the remaining surgeries.
Similar refraction but lower visual acuity in post-vitrectomy eyes
Dr Chiras and his associates observed no significant difference between the refractive outcomes of the two groups. Three weeks after surgery, refraction was within 1.0D of target in 88.6% of the prior vitrectomy group and 89.8% of the reference group.
Refraction was within 0.5D in 65.8 % of the prior vitrectomy group and in 63% of the reference group.
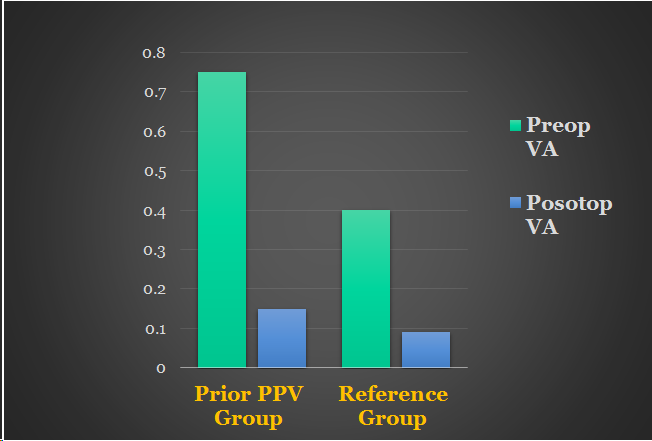
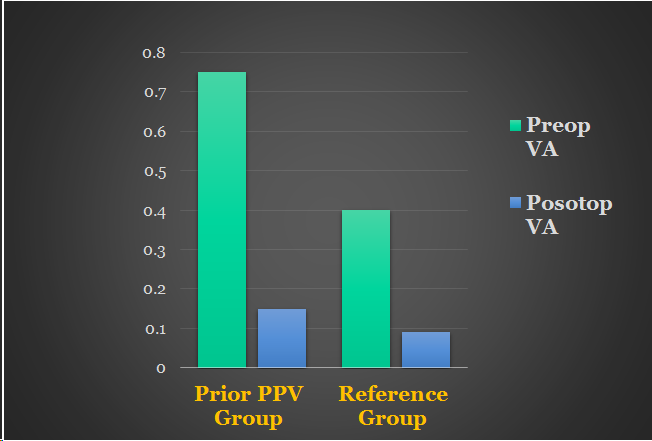
However, vitrectomised eyes had significantly worse preoperative and postoperative visual acuity than the non-vitrectomised eyes, which was related to the pre-existing retinal pathology requiring vitrectomy, Dr Chiras said.
The preoperative logMAR visual acuity in eyes that had undergone previous vitrectomy was 0.7 compared to 0.4 in the reference group (p<0.0001) and the postoperative visual acuity was 0.15 vs 0.09 (p=0.014).
On the other hand, postoperative visual acuity was 6/12 or better in 79.9% of the prior vitrectomy group and 89.3% in a reference group. Furthermore, postoperative visual acuity was improved compared to preoperative values in 96.6% of the prior vitrectomy group and 91.4% of the controls.
More CME and PCO in vitrectomised eyes
Regarding intraoperative complications, there were two (1.3%) cases of zonular dialysis in the prior vitrectomy group, seven (1.1%) cases of anterior capsule tear and six (1%) cases of capsule rupture in the non-vitrectomy group.
During follow-up there was a higher incidence of postoperative cystoid macular oedema (4% vs 1.5%, p=0.046) in the vitrectomised eyes. The rate of posterior capsule opacification was significantly higher in vitrectomised eyes (6% vs 0.7%, p<0.0001).
The vitrectomised eyes also had a higher incidence of postoperative ocular hypertension (1.3% vs 0.2%) and retinal detachment (1.3% vs 0%), but a lower incidence of anterior uveitis.
“A close postoperative follow-up is recommended for vitrectomised eyes, considering the higher incidence of cystoid macular oedema and posterior capsule opacification. Prospective studies including randomised controlled trials could help to analyse the relationship between previous vitrectomy and the development of cystoid macular oedema after cataract surgery and identify possible prophylactic options to reduce this risk,” Dr Chiras said.
Dr Chiras noted that cataract surgery in post-vitrectomised eyes has become more common in recent years. However, it is challenging and the percentage of eyes achieving postoperative vision greater than 6/12 has varied in previous studies. There are also contradictory reports regarding the safety of phacoemulsification in vitrectomised eyes.
LIMITATIONS OF THE STUDY
Limitations of the present study were that it was retrospective, used Snellen visual acuities to calculate logMAR visual acuity and had different durations of follow-up, Dr Chiras said.
“Based on our results, we can say that although cataract surgery is challenging, with careful consideration of multiple factors before, during and after surgery, an experienced cataract surgeon can adapt their technique to avoid complications and ensure the safest outcomes. However, the underlying pathology and other factors may compromise visual outcomes,” he concluded.
Dimitrios Chiras: d.chiras@nhs.net

 LogMAR Visual Acuity outcomes
LogMAR Visual Acuity outcomes
 Dimitrios Chiras MD, PhD, FEBO
Dimitrios Chiras MD, PhD, FEBO