Bringing OCT-A to the bedside
Hand-held probe enables imaging in awake neonates

Cheryl Guttman Krader
Published: Tuesday, July 9, 2019
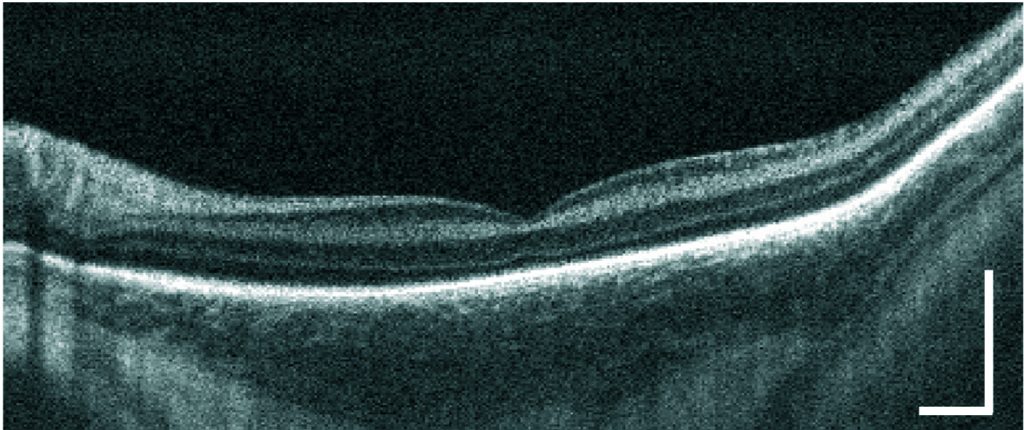 Typical OCT B-scan from an infant at 28-week gestational age. White bar = 0.5mm[/caption]
Initial clinical experience with an investigational handheld swept-source optical coherence tomography angiography (OCT-A) device suggests it has the potential to become a new diagnostic tool for retinopathy of prematurity (ROP), according to researchers who presented their findings at the 2019 annual meeting of the Association for Research in Vision and Ophthalmology (ARVO) in Vancouver, Canada.
“This is the first report showing successful OCT-A imaging in awake, premature infants in the neonatal intensive care unit,” said Ruikang Wang PhD, Professor of Bioengineering and Ophthalmology, University of Washington, Seattle, USA.
“Our prototype, however, still has some limitations, and we are working to make modifications that will address those issues.”
The miniature SS OCT-A device is designed to make the examination easy for the operator and safe and comfortable for the infant. It is light in weight (<1kg) and features an on-probe display along with a live pupil-finding video that provides feedback to facilitate probe positioning. It is non-invasive, can be used without an eyelid speculum or sedation and provides rapid image capture. The prototype has an imaging speed of 200kHz and each volume is acquired in less than five seconds with an approximately 30° field-of-view.
[caption id="attachment_15657" align="alignleft" width="1024"]
Typical OCT B-scan from an infant at 28-week gestational age. White bar = 0.5mm[/caption]
Initial clinical experience with an investigational handheld swept-source optical coherence tomography angiography (OCT-A) device suggests it has the potential to become a new diagnostic tool for retinopathy of prematurity (ROP), according to researchers who presented their findings at the 2019 annual meeting of the Association for Research in Vision and Ophthalmology (ARVO) in Vancouver, Canada.
“This is the first report showing successful OCT-A imaging in awake, premature infants in the neonatal intensive care unit,” said Ruikang Wang PhD, Professor of Bioengineering and Ophthalmology, University of Washington, Seattle, USA.
“Our prototype, however, still has some limitations, and we are working to make modifications that will address those issues.”
The miniature SS OCT-A device is designed to make the examination easy for the operator and safe and comfortable for the infant. It is light in weight (<1kg) and features an on-probe display along with a live pupil-finding video that provides feedback to facilitate probe positioning. It is non-invasive, can be used without an eyelid speculum or sedation and provides rapid image capture. The prototype has an imaging speed of 200kHz and each volume is acquired in less than five seconds with an approximately 30° field-of-view.
[caption id="attachment_15657" align="alignleft" width="1024"]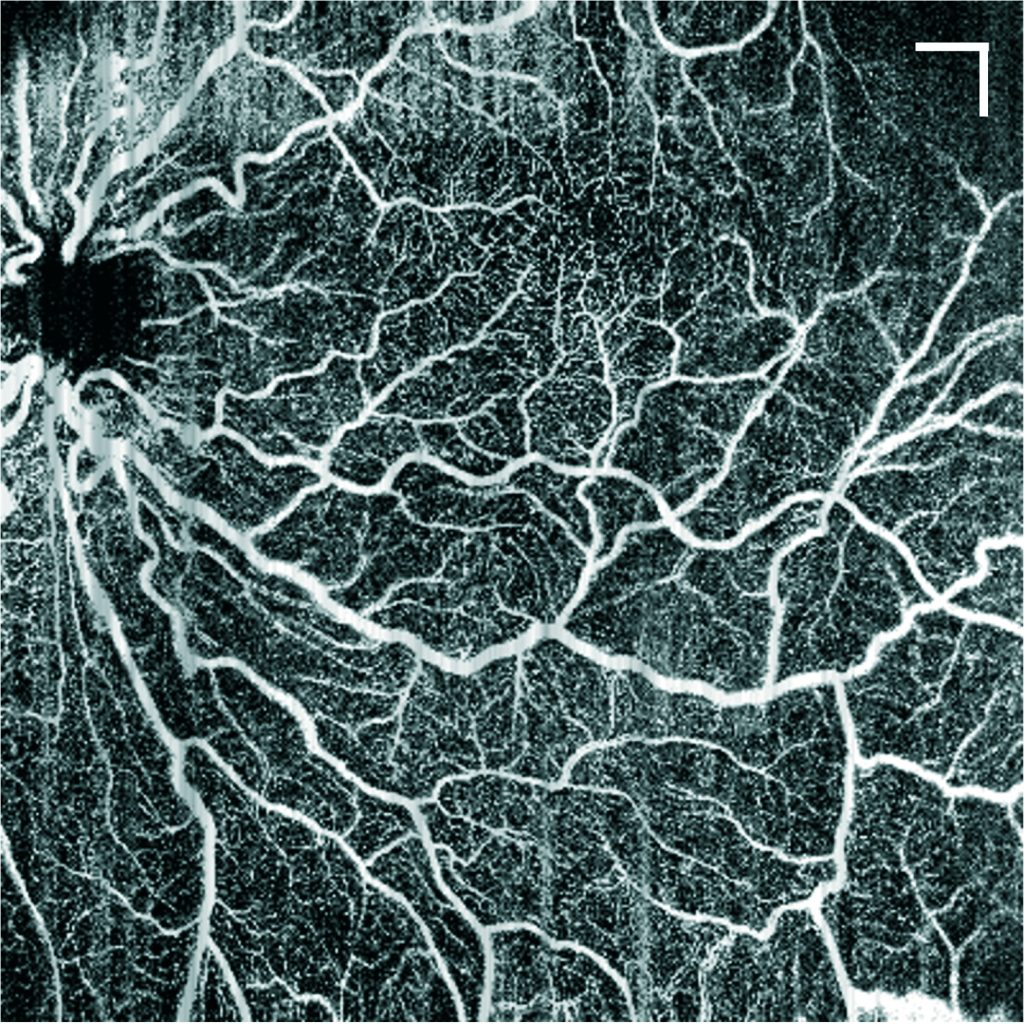 Wide field retina SS-OCTA captured from an awake infant at 28-week gestational age with retinopathy of prematurity. White bar = 0.5mm[/caption]
To assess the performance of the device for providing high resolution images, Yasman Moshiri BS, a University of Washington medical student, evaluated images obtained in eight premature infants (mean gestational age 27.3 weeks) who were undergoing routine ROP screenings at the University of Washington Medical Center Neonatal Intensive Care Unit. The images were acquired with the infants lying on their back. Each infant was imaged between one and six times, for a total of 19 imaging sessions.
Images were considered to be “good quality” if detailed microvasculature could be visualised in at least one retinal layer without significant motion artefact or defocus. The review showed good quality images were obtained of the foveal microvasculature in 11 (58%) of the imaging sessions for six (75%) infants and of the peripapillary microvasculature in 14 (74%) imaging sessions for five (63%) infants.
“The majority of the images were of sufficient quality to screen for pathology, and we hope that we can implement the use of this device in other settings,” said Ms Moshiri.
Ongoing efforts to improve the device include reconfigurations to increase the field-of-view.
“Although the largest field-of-view provided by our system is regarded as ‘wide-field’, it is not large enough to cover the peripheral retina where there are essential characteristics of ROP,” said Dr Wang.
Ruikang Wang: wangrk@uw.edu
Wide field retina SS-OCTA captured from an awake infant at 28-week gestational age with retinopathy of prematurity. White bar = 0.5mm[/caption]
To assess the performance of the device for providing high resolution images, Yasman Moshiri BS, a University of Washington medical student, evaluated images obtained in eight premature infants (mean gestational age 27.3 weeks) who were undergoing routine ROP screenings at the University of Washington Medical Center Neonatal Intensive Care Unit. The images were acquired with the infants lying on their back. Each infant was imaged between one and six times, for a total of 19 imaging sessions.
Images were considered to be “good quality” if detailed microvasculature could be visualised in at least one retinal layer without significant motion artefact or defocus. The review showed good quality images were obtained of the foveal microvasculature in 11 (58%) of the imaging sessions for six (75%) infants and of the peripapillary microvasculature in 14 (74%) imaging sessions for five (63%) infants.
“The majority of the images were of sufficient quality to screen for pathology, and we hope that we can implement the use of this device in other settings,” said Ms Moshiri.
Ongoing efforts to improve the device include reconfigurations to increase the field-of-view.
“Although the largest field-of-view provided by our system is regarded as ‘wide-field’, it is not large enough to cover the peripheral retina where there are essential characteristics of ROP,” said Dr Wang.
Ruikang Wang: wangrk@uw.edu
Tags: optical coherence tomography angiography (OCT-A), retinopathy of prematurity (ROP)
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.