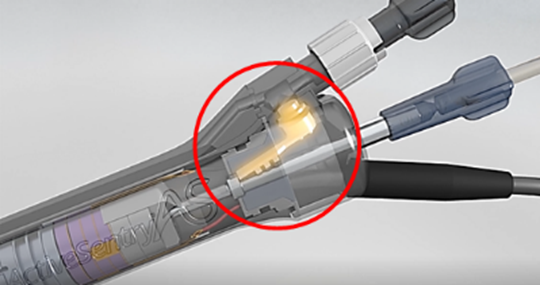
Sensing Improved Phaco Safety
Handpiece with dynamic IOP sensor protects against occlusion surge. Dermot McGrath reports

Howard Larkin
Published: Tuesday, August 31, 2021
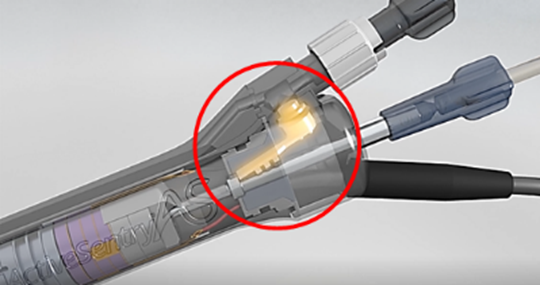
Handpiece with dynamic IOP sensor protects against occlusion surge. Dermot McGrath reports

Published: Tuesday, August 31, 2021