Cornea, Refractive Surgery, Refractive
Minimising Corneal Damage in Laser Refractive Surgery
SMILE leaves the cornea more intact, but LASIK may be preferred for many patients. Howard Larkin reports.

Howard Larkin
Published: Thursday, December 1, 2022
Corneal damage is a significant risk of laser refractive surgery, leading to complications such as dry eye, corneal haze, and even ectasia. Vance Thompson MD and H Burkhard Dick MD, PhD debated the merits of laser in situ keratomileusis (LASIK) versus small incision lenticule extraction (SMILE) for minimising corneal damage in the Journal of Cataract and Refractive Surgery Symposium at the 40th Congress of the ESCRS in Milan.
Arguing for LASIK, Dr Thompson noted while he does LASIK and SMILE as well as photorefractive keratectomy (PRK), SMILE is likely the procedure of the future. Nonetheless, LASIK, particularly wavefront-guided and topography-guided procedures, is safe for most patients and still offers optical advantages that make it preferable for many.
“I do PRK, LASIK, and SMILE, and I am a fan of all three.”
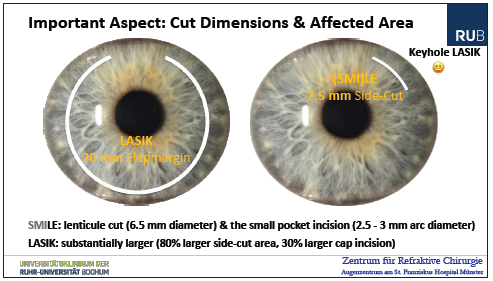
Regarding minimising corneal damage, LASIK reduces risk of a decentred ablation because it is easier and more reliable to achieve precise centration with patient fixation than suction femtosecond laser docking required for SMILE. Though, Dr Thompson noted the difference may wane as SMILE docking and tracking technology improves.
When doing SMILE, “I tell patients if we can’t centre the laser, we are going to cut a flap and do LASIK,” Dr Thompson said. “As my experience with SMILE has increased, this has become a very rare event. My comfort with centring SMILE has increased with my experience.”
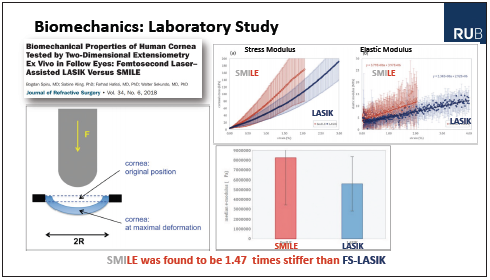
The procedure also reduces the surgeon’s learning curve and related intraoperative risk. When retreatment is necessary, LASIK allows for it using the same technology, while SMILE retreatment usually requires switching to LASIK or PRK. However, SMILE is superior for reducing dry eye risk, preserving corneal surface sensitivity, and preventing flap dislocation due to postoperative eye trauma. SMILE also preserves the biomechanical integrity of the cornea, though ectasia is still a risk, Dr Thompson allowed.
Beyond corneal damage, LASIK is superior for treating hyperopia, low myopia, and cylinder, as well as visually significant higher-order aberrations and topographic irregularities such as when topographic cylinder and manifest cylinder diverge, he noted. Some studies show that wavefront-guided LASIK may also yield slightly better visual acuity and contrast sensitivity.
“LASIK wins on fixation—when there is a need for topo-guided or wavefront-guided surgery, when there is low cylinder. … SMILE wins when the correction [it can provide] is ‘high enough’, where there is dry eye concern, where topo-or wavefront-guided are not needed, or where trauma is a risk. If correction is optimal and centred well, SMILE is my preferred lamellar approach, with these exceptions,” Dr Thompson concluded.
LENTICULE EXTRACTION
Advocating for SMILE, Dr Dick noted that “lenticule extraction” (LE) is a better generic term to avoid confusion with similar procedures competing with SMILE, which is a trademark of Carl Zeiss Meditec, including CLEAR (Ziemer), SmartSight (Schwind), and SILK (Johnson & Johnson).i
Beyond the obvious patient appeal of a smaller incision “keyhole” surgery, several studies have shown lenticule extraction surgery preserves corneal strength better than LASIK, Dr Dick noted. Corneal hysteresis, or the ability to rebound after impact, is also greater after lenticule extraction than LASIK—out to three years.
Dry eye inflammatory factors—including MMP-9 and cytokines—also lessen after lenticule extraction than after LASIK, while CGRP, a tear film factor that helps maintain the corneal epithelium, reduces after LASIK, Dr Dick observed. This reduction relates to a further jump in ocular surface disease index (OSDI) scores and reduced tear film break-up time after LASIK compared with lenticule extraction. Nerve damage also increases in LASIK than lenticule extraction, with sensation better immediately after surgery, even after six months in some studies.
At the same time, Dr Dick said visual outcomes for myopic patients have been excellent with lenticule extraction. The few studies comparing LE with wavefront-guided LASIK that have found better 20/20 results with LASIK, he noted, have compared outcomes for early or suboptimal iterations of LE. More recently, larger studies using optimised laser energy and spot placement as well as improved surgical instruments and techniques have improved the percentage of LE patients corrected to 20/20 or better.
Lenticule extraction complication rates are also low, Dr Dick said. In one large study, suction loss occurred in 0.46% of patients, though all completed surgery. Small lenticule remnants were left behind in 0.11% of cases, but these were also managed intraoperatively. Induction of irregular astigmatism occurred in a few cases, indicating a need to convert to LASIK.ii
“There is evidence that lenticule extraction causes less dry eye disease and other ocular surface problems, leaves more corneal nerves intact, is better for corneal biomechanics, and provides comparable, excellent results. For me, it is the best option for patients,” Dr Dick concluded.
In 2021, Dr Thompson reported doing about 15% PRK, 20% SMILE, and 65% Femto-LASIK procedures, while Dr Dick reported 15% PRK, 15% LE, and 70% Femto-LASIK. When asked which they would choose for themselves as a younger person, both felt it was a tough decision but chose Femto- LASIK, assuming no ongoing corneal difficulties.
But that could change. “SMILE is a procedure in evolution; it is an elegant procedure, and a modern-day refractive surgeon needs to have the ability to do SMILE-type procedures,” Dr Thompson said.
i-ii Reinstein D, Archer T, et al. Journal of Refractive Surgery, 2022.
Vance Thompson MD is founder of Vance Thompson Vision and professor of ophthalmology at the University of South Dakota Sanford School of Medicine, both in Sioux Falls, South Dakota, US. vance.thompson@vancethompsonvision.com
H Burkhard Dick MD, PhD is full clinical professor of ophthalmology and Chairman at Ruhr University Eye Hospital, Bochum, Germany. DICKBurkhard@aol.com
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.