Cornea
Amniotic Membrane Transplantation for Ocular Surface Disease
Study demonstrates differences among surgical indications

Cheryl Guttman Krader
Published: Monday, July 3, 2023
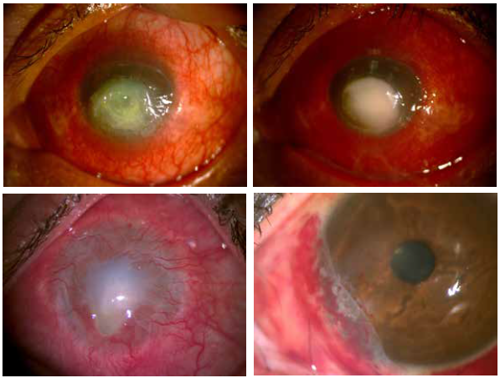
Amniotic membrane transplantation (AMT) is useful for treating ocular surface diseases (OSDs), a large retrospective review confirms.
“Our research highlights AMT as a safe and effective procedure for managing many conjunctival and corneal pathologies, but also that desired results were achieved in lower percentages of eyes with ocular burns, ocular surface reconstruction, and limbal stem cell deficiency (LSCD),” said Dr Naomi C Zatarain Barrón.
“Further research is needed to determine why the results were poorer when AMT was used for the latter applications. We hope the findings might help guide decisions about when we should consider alternate strategies or continue to use AMT because it is safe and the best intervention currently available.”
The study included 246 eyes of 215 patients who underwent AMT for OSD between January 2017 and October 2022. The patients had a mean age of 48 years, and mean available follow-up was almost 11 months. Pterygium was the leading indication for AMT (37.8%), followed by perforation (15.0%), burns (12.2%), neoplasms (11.4%), ocular surface reconstruction (10.2%), epithelial defect/ulcer (8.1%), and LSCD (5.3%).
Cryopreserved amniotic membrane was used for the procedure, which proceeded without any complications in all but two cases. Postoperative complications occurred in 110 eyes (44.7%), with pterygium recurrence the most common (20.0%). Other postoperative complications were symblepharon (18.2%) and epithelial defect (11.8%). Analysed IOP data showed no significant difference between the preoperative and postoperative levels.
“We did not have a reason to suspect a shift in IOP after AMT, but we analysed this endpoint to be comprehensive in our evaluation of safety,” Dr Zatarain said.
Overall, AMT was associated with a statistically significant improvement in BCVA and UCVA: BCVA improved from 1.16 logMAR preoperatively to 0.94 logMAR postoperatively, and UCVA improved from 1.33 preoperatively to 1.14 logMAR postoperatively.
The desired postoperative result—defined with criteria that varied depending on the indication—was achieved in 100% of eyes that underwent AMT for management of neoplasm, in 80% with an epithelial defect/ulcer, 76.3% with pterygium, and 73.0% with a perforation. However, only 60.0% of eyes with an ocular burn, 52.0% of those requiring ocular surface reconstruction, and 38.5% of those with LSCD achieved the desired result after AMT.
For a better understanding of the lower success rates using AMT in eyes with ocular burns, LSCD, or those needing ocular surface reconstruction, Dr Zatarain and colleagues plan to conduct additional analyses looking for specific factors that might predict a positive outcome.
“We would like to conduct subgroup analyses,” she told EuroTimes. “For example, for our patients with LSCD, we will stratify them based on the underlying cause for the LSCD to see if the aetiology was a prognostic factor.”
Dr Zatarain presented this study at ARVO 2023 in New Orleans, Louisiana, US.
Naomi Carolina Zatarain Barrón MD is an ophthalmology resident at Instituto de Oftalmología Fundación Conde de Valenciana IAP, Mexico City, Mexico. naomiztnb@gmail.com
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.