Cornea
Unleashing OCT’s Full Potential
Performance of newest tool for corneal evaluation meets or beats older standard technologies.

Cheryl Guttman Krader
Published: Monday, April 1, 2024
Optical coherence tomography (OCT) corneal imaging is a unique and powerful diagnostic tool with utility already documented in several applications. Its capabilities are expected to enhance in the near future, pending approval of more advanced features and new platforms offering even higher performance, according to David Huang MD, PhD, who co-invented OCT technology in 1991.
“Corneal OCT is a relatively new tool that is now hitting the mainstream after several devices received marketing clearance from the US FDA,” Dr Huang said. “My hope is more clinicians will begin using this technology that gives a comprehensive evaluation of the cornea and is the only noncontact modality for corneal imaging that can resolve the epithelium.”
Functions and applications
OCT corneal mapping generates four types of maps—anterior topography, posterior topography, epithelial thickness, and pachymetry. Its current applications include measurement of total (net) corneal astigmatism through its ability to measure astigmatism of the cornea’s anterior and posterior surfaces.
Dr Huang noted the possibility of mapping corneal topography with OCT became a reality with the advent of higher-speed imaging. Following implementation of a motion detection algorithm to remove motion error and improve repeatability, research he conducted with co-workers showed the maps generated by corneal OCT agreed well with those provided by current standards (e.g., Scheimpflug imaging).
Additional research evaluating corneal OCT for measuring net corneal astigmatism showed it had greater repeatability and accuracy than Scheimpflug imaging when the two techniques were used in patients with keratoconus and post-LASIK pseudophakic patients implanted with a non-toric IOL and compared to the patients’ refraction as the reference standard.
Differential diagnosis of corneal steepening represents another application of corneal OCT, where its ability to detect ectasia and differentiate it from other corneal irregularities is done based on the topography, pachymetry, and epithelial thickness maps. Dr Huang explained that the epithelium is generally thinner at sites of focal steepening in eyes with ectasia but tends to be thicker at sites of focal steepening related to other causes, such as dry eye disease, basement epithelial membrane dystrophy, or contact lens-related warpage.
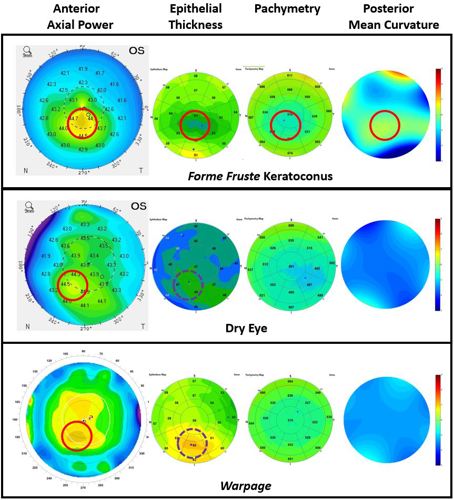
“This concept relates to the fact that there is secondary modulation of epithelial thickness along with coincident thinning at the site of thickening in ectasia or keratoconus. In contrast, steepening related to primary epithelial deformation (i.e., warpage) is caused by focal epithelial thickening,” he said.
“In addition, the steepening in keratoconus is inferotemporal and associated with a concentric pattern of epithelial thinning.”
Dr Huang reported that by using the pattern recognition features he described along with other quantitative parameters, corneal OCT performed at a very high level of accuracy, provided near-perfect recognition of subclinical keratoconus, and showed good sensitivity for detecting forme fruste keratoconus.
Case examples involving patients being screened for refractive surgery or having a corneal irregularity post-LASIK demonstrated how the corneal OCT’s algorithm could determine if steepening was associated with ectasia, a steep central island, or epithelial deformation.
Dr Huang spoke at AAO 2023 in San Francisco, US.
David Huang MD, PhD is Professor of Ophthalmology and Biomedical Engineering, OHSU School of Medicine and Wold Family Chair in Ophthalmic Imaging, OHSU Casey Eye Institute, Portland, Oregon, US. huangd@ohsu.edu
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.