Planning effective patient pathways
Maximising patient flow in a busy refractive clinic starts before patients arrive

Rod Solar
Published: Friday, June 21, 2019
 Rod Solar, Practice Development Consulting Director, LiveseySolar
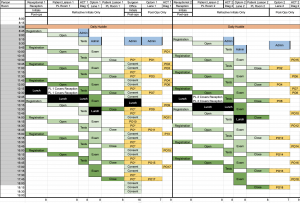
I’m excited to welcome Arthur Cummings to the Practice Development Workshop that I’ll be moderating at the 37th Congress of the ESCRS this September. In Paris, he will present a session called “Optimising Patient Flow in a Busy Practice”. Having consulted in busy refractive settings for the past 20 years (including Mr Cummings’ practice), I have accumulated a wealth of experience in planning effective patient pathways - especially before patients have surgery. In this article, I share my top tips for maximising your patient flow before and during first appointments.
Rod Solar, Practice Development Consulting Director, LiveseySolar
I’m excited to welcome Arthur Cummings to the Practice Development Workshop that I’ll be moderating at the 37th Congress of the ESCRS this September. In Paris, he will present a session called “Optimising Patient Flow in a Busy Practice”. Having consulted in busy refractive settings for the past 20 years (including Mr Cummings’ practice), I have accumulated a wealth of experience in planning effective patient pathways - especially before patients have surgery. In this article, I share my top tips for maximising your patient flow before and during first appointments.