Cornea
In the Know—Iris Repair, Part 3
The third of this multi-part series reveals key techniques no surgeon should pass.
Soosan Jacob
Published: Friday, March 1, 2024
Iridodialysis refers to a separation of the iris from the ciliary body at the iris root. It can be post-traumatic or iatrogenic. Small iridodialysis, especially if covered by the upper lid, may be ignored, but larger dialysis can cause visual symptoms such as glare, photophobia, and monocular polyopia. It also causes polycoria and often results in a displaced pupil. In light-coloured irides, it causes cosmetic concerns as well.
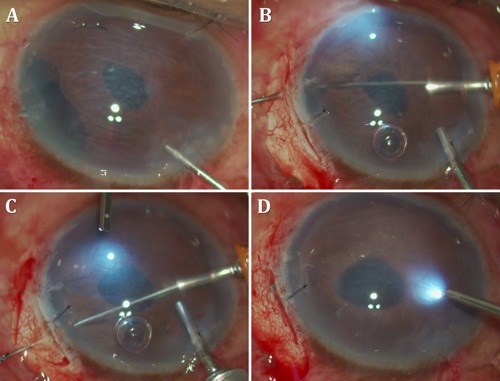
Contemporary iridodialysis techniques
When suturing the iris back, the first step is to make a peritomy and create a scleral groove about 1.5 mm behind the limbus. Next, the anterior chamber (AC) is filled with viscoelastic, and the iris straightened out with all folds removed and brought to lie in the final intended position, using a double-armed 10-0 prolene suture with two long, thin, and preferably curved needles (CIF-4, Ethicon) on either side. A paracentesis is made on the side opposite to iridodialysis, and one of the needles is passed carefully through the paracentesis into the iris near the dialyzed root and docked into a 30-gauge needle passed through the scleral groove, then railroaded out through the sclera. The second needle is then passed through the iris stroma about one clock hour away from the previous pass and again railroaded into a needle passed through the scleral groove radial to it and a short distance away from the first one.
Care should be taken to ensure a free loop between the two needles. Once both needles have been externalized, they are pulled, drawing the loop into the AC and against the iris. The externalized sutures are then cut and tied down to appose the iris against the scleral wall. Overtightening the prolene suture can occur easily, so the knots should be tightened carefully. Multiple such passes of double-armed prolene suture are required for a large dialysis area. The knots are pushed deep into the scleral groove, and the conjunctiva is closed. A partial thickness scleral flap is sometimes used instead of a scleral groove to avoid exposed knots.
Hoffman pocket
The scleral groove technique can result in exposed knots—leading to the introduction of the Hoffman pocket to avoid this problem. A tunnel is created backwards from the limbus into the sclera, and the two needles of the double-armed suture exit through the roof of this pocket. These are then cut and withdrawn from within the pocket by pulling them out with a rod or Sinskey hook. Tying the two ends of the suture buries the knot within the tunnel. This technique has the added advantage of not requiring any conjunctival peritomy.
Scleral tunnel
A technique similar to the Hoffman pocket, this follows a conjunctival peritomy with the creation of a scleral tunnel starting about 2.0 mm posterior to the limbus. The needles are externalized from the roof, and the cut suture ends are pulled out through the scleral pocket and tied within it. This method has the disadvantage of needing a conjunctival peritomy. If a scleral tunnel is already created for some other purpose—e.g., rigid IOL explantation or manual small incision cataract surgery—an underlying iridodialysis can be sutured to the scleral tunnel floor.
Hang-back technique
An overtightened knot can result in an updrawn pupil. In the hang-back technique, the double-armed sutures are tied down with enough slack to give a cosmetically and visually ideal outcome. The non-appositional closure results in an iris literally hung back from the sclera.
Trocar-assisted iridodialysis repair
Take care passing the needles into the AC to avoid snagging onto corneal fibres at the paracentesis—which results in the prolene suture catching at the incision and not being able to be pulled freely into the AC. Such a situation necessitates cutting the suture and restarting. A simple modification, described by Dr Amar Agarwal, uses a trocar passed through the paracentesis. Passing the double-armed needles through the trocar removes any chance of the needle accidentally engaging corneal tissue during its passage. The trocar can be removed once the loop lies free within the AC.
Cobbler’s technique
This technique allows easy and rapid repair of the entire iridodialysis through a small incision and without repeated entry and exit or AC shallowing. One end of a 10-0 prolene suture is threaded through a 26- or 27-gauge needle, which then passes from a diametrically opposite paracentesis into the AC to take a bite of the iris periphery and exit through a slanting scleral groove. The cut end of the suture is retrieved outside the eye while the needle is again internalized, only to be passed through an adjacent part of the iris and scleral groove. This time, a loop of suture is retrieved, and the needle reinternalized. This repeats as many times as required to cover the entire dialyzed iris, creating multiple loops. The initial free end is then passed through all loops except the last one and tied down to the cut end of the last loop. Cobbler’s technique requires only one knot instead of multiple knots.
Rivet technique
The cut end of a 6-0 prolene suture is flanged using a low-temp cautery. A 26-gauge needle then passes through the sclera and the dialyzed iris periphery. The free end of the suture passes into the needle, and the needle withdrawn. The flanged end apposes against the iris and pulls it towards the scleral wall. The other end is trimmed sufficiently and also flanged to ensure iris apposition and the flange burial in the sclera.
Flanged repair
Two ends of a 6-0 prolene suture are passed through the peripheral iris and out through the sclera. Both ends are drawn so the internal loop brings the iris against the sclera, then flanged with a low-temperature cautery and buried in the sclera.
Soosan Jacob MS, FRCS, DNB is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.