Multifocal IOLS and Beyond
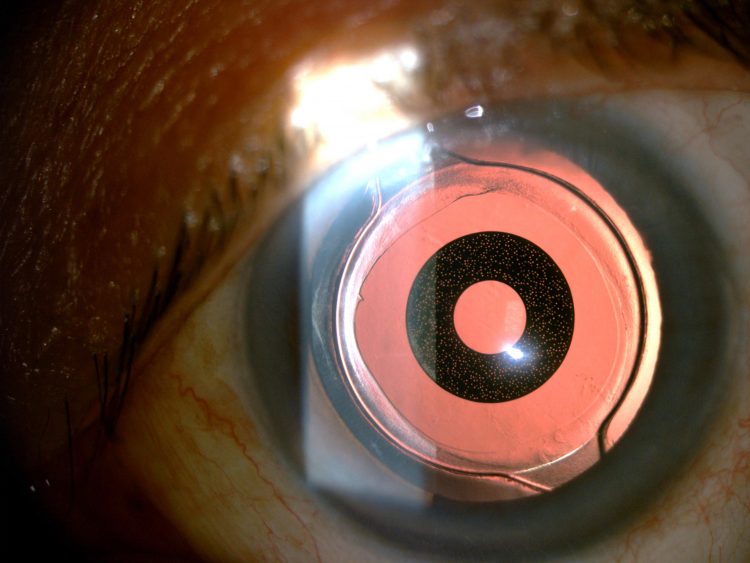
AcuFocus IC-8 small-aperture IOL. Courtesy of Robert Edward Ang MD
A functional accommodative intraocular lens (IOL) may exist somewhere in the future, but meanwhile presbyopic patients in the present would like to have functional vision at more than one distance. The new wave of multifocal and extended depth of focus (EDOF) IOLs are helping overcome some of the existing limitations to current presbyobic IOL solutions.
A wide variety of lenses that leverage static optical principles to address presbyopia are now available or close to market. These include multifocal lenses that provide two or three focal depths, as well as lenses that employ diffraction, a small aperture, spherical aberration or polyfocality to smoothly extend depth of focus. Monovision, using monofocal lenses of differing powers or to enhance the effect of newer EDOF lenses, also remains a viable solution.
But physics is a harsh taskmaster. Dividing or stretching the focal point of light entering the eye inevitably involves trade-offs. Generally speaking, seeing clearly at more than one distance comes at the cost of reduced contrast sensitivity, low-light vision and uncorrected visual acuity at all distances – as well as glare, halos, starbursts and sundry dysphotopsia.
Some of these trade-offs are evident in objective tests of presbyopia correcting IOL optics, such as wavefront and point spread analyses. Some also appear in subjective defocus curves and contrast sensitivity tests, and functional tests such as reading speed.
How they will play out in a given patient is another matter. The anatomy and neurophysiology of human vision makes some aberrations easier to cope with than others – and this capacity varies by individual. Also variable is patients’ willingness to put up with a given trade-off, such as better reading vision for limited night driving. And some effects that are vital to everyday function, such as speed of shifting focus and depth perception, are difficult to test, said Ioannis G Pallikaris MD, PhD, of the University of Crete, Greece. He suggests that standardised tests be developed for lens performance to enable comparisons.
For best results, the trade-offs of various static presbyopic IOLs, gleaned from both specifications and clinical experience, must be matched to individual patient needs, according to surgeons experienced with a range of options. Below are some of the major static optic types and how they perform.
MULTIFOCALS MADE MANAGEABLE
Multifocal IOLs address presbyopia by splitting incoming light into two or three distinct focal points, typically with a near add of 2.5D to 4.0D, with a third intermediate step for trifocals. With their high near add, multifocals generally provide good reading vision, leading to more patients reporting complete spectacle independence than with monofocal or even newer EDOF lenses.
The trade-off is image quality. Splitting light means that less light is available to produce an image at any given distance. This translates to reduced contrast sensitivity. That an out-of-focus image is also superimposed further increases blur, while the complex diffractive or refractive optics needed to produce multifocality also tend to scatter light, producing dysphotopsia.
This trade-off is well documented, noted Oliver Findl MD, of Hanusch Hospital, Vienna, Austria. He cited a meta-analysis of 16 masked randomised controlled trials involving more than 1,600 patients that found multifocal lenses improved near vision and spectacle independence compared with monofocals, but multifocals also reduced contrast sensitivity, and were twice as likely to produce annoying or disabling glare and dazzle (Calladine D et al. Cochrane 2012).
Dr Findl has seen similar results in his own research, along with higher rates of explants for multifocal lenses (Wilkins MR et al. Ophthalmology. 2013;120(12): 2449–2455). Indeed, the number of explanted multifocal lenses reported through the ESCRS/ASCRS online survey has grown for the last several years, with the vast majority removed because of glare and other dysphotopsia.
However, some newer multifocal IOL designs address these issues, said Jorge L Alió MD, PhD, of Vissum Ophthalmologic Institute, Alicante, Spain. His tests show that the Zeiss AT LISA trifocal and trifocal toric lenses provide better contrast sensitivity at all spatial frequencies than several other multifocals he implants, with values close to a monofocal (Mojzis P, Alio JL et al. JCRS 2014;40:60-69. JCRS in press). Glare is also less than earlier lenses, which he attributes to advanced optic design, which Zeiss says reduces light scatter and photic effects by smoothing transitions between optic zones on the lens.
AT LISA tri is an 11.0mm single-piece plate haptic design with a 6.0mm diffractive optic with adds of +3.33D for near and +1.66D for intermediate composed of a hydrophilic acrylic with hydrophobic surface. Dr Alió pointed out the its defocus curve lacks the pronounced dip at intermediate distances of bifocal IOLs, mimicking the defocus performance of a functional human eye. He considers this an important indicator of real-world lens performance as defocus is a function of neuroprocessing as well as lens optics. “It correlates well with the quality of vision as perceived by the patient in terms of multifocality,” he said.
Dr Findl also finds the AT LISA trifocal, along with the FineVision trifocal, to be tolerated better than bifocal IOLs. He will implant them in a hyperopic patient but is reluctant to do so in emmetropic or myopic patients. “They are used to good quality near vision and often don’t do well with a multifocal,” he said. He also cautions that reduced contrast sensitivity can be a problem for patients who later develop retinal issues.
DIFFRACTIVE EDOF
Extended depth of field IOLs offer another presbyopic solution. One such lens is the Tecnis Symfony (Abbott Medical Optics). Compared with a similar aspheric monofocal lens, the Symfony lens’ diffractive echelette optic elongates its focal point by approximately 1.75 dioptres, according to a recent clinical study by Joseph JK Ma MD, FRCSC, of the University of Toronto, Canada. This improves visual acuity continuously across the defocus curve, yielding binocular vision of 20/25 or better over approximately -2.5D of defocus when extended with micromonovision targeting -0.75D in the non-dominant eye. This also results in excellent binocular intermediate stereo vision from the bilateral overlapping defocus curves.
The Symfony also corrects for chromatic aberration, improving contrast sensitivity, which is comparable to a monofocal lens. However, the most significant trade-off is less near vision when compared with multifocals IOLs.
It’s a trade-off many patients are more willing to make in order to minimise the compromise in the quality of their distance vision, said Dr Ma. In his first 85 Symfony patients, contrast sensitivity, glare and halos were similar to those seen with monofocal lenses, while providing intermediate and even reading vision when combined with mini-monovision. However, the lens is not entirely without symptoms, and there can still be unique night-time symptoms associated with the lens, such as a web-like effect associated with red lights, that appears in some patients, does not appear to be debilitating, and improves dramatically with time.
Although the effect can be different between patients, in addition to providing 20/20 vision up to -2.0D defocus in some patients, the lens is very forgiving of astigmatism, Dr Ma said. He implanted one in a lens exchange in a pseudophakic patient with forme fruste keratoconus. Despite some asymmetric astigmatism, the eye had 20/25 uncorrected distance vision with spherical equivalent tolerance up to -1.75D, allowing her to both drive and read a computer monitor easily without glasses.
Even more importantly, the patient was as satisfied with the quality of vision in the EDOF lens as with the previous monofocal in that eye as well as the monofocal in the fellow eye, Dr Ma said. “As beautiful as the defocus curve looks, we want to see how it performs in the real world.” In this case, well enough that the patient subsequently referred her mother.
SMALL APERTURE EDOF
The IC-8 IOL (AcuFocus) extends depth of focus using the pinhole effect, incorporating a 3.2mm diameter mask with a 1.36mm central aperture on a 6.0mm one-piece hydrophobic acrylic lens. This broadens the defocus curve on both sides of the focal point, resulting in vision of 20/32 or better over about -2.0D defocus when targeted for plano distance vision, said Robert Edward Ang MD, Manila, The Philippines. Minimonovision broadens that to about -3.0D, Dr Ang said. Stereopsis is also achieved over a range of distance.
In a study of 16 patients implanted in the non-dominant eye targeting plano distance, mean uncorrected binocular distance vision was 20/20, intermediate 20/25, and near J2 or about 20/25 12 months post-op, Dr Ang said. The trade-off is a slight reduction in distance visual acuity (no more than one line) and a small loss of contrast sensitivity in the IC-8 implanted eye, about 0.1 to 0.2 log units compared with the monofocal fellow eye.
However, the loss of night contrast sensitivity is not enough to affect patients’ function, Dr Ang said. Due to less glare and halos, night vision is better than with trifocal IOLs he also implants, and is good even in 10 patients implanted bilaterally with the IC-8. “One of them rides a motorcycle at night,” Dr Ang said. However, the IC-8 does not provide as much near add as the trifocals.
The current lens design requires an incision of about 3.0mm, said Dr Ang. However, the pinhole optic is more forgiving of refractive error due to the uninterrupted depth of focus and even tolerates up to 1.50 D of astigmatism.
The mask raises questions about viewing the retina, but it is possible to see around it to do any kind of retinal exam and to perform surgical procedures, Dr Ang said. Likewise, he has performed posterior capsulotomies on patients with no issues.
ADJUSTABLE SPHERICAL ABERRATION EDOF
Inducing spherical aberration in the lens is yet another way of extending depth of focus. This can be done with the Light Adjustable Lens (LAL, Calhoun Vision). This three-piece IOL with 6.0mm optic is constructed of ultraviolet-sensitive silicone polymers that allow spherical and toric adjustment of about 2.0D as well as correction of aberrations using a special lamp. With the dominant eye at emmetropia, inducing -0.23 microns of spherical aberration in the non-dominant eye improved intermediate range vision to 0.94 or nearly 20/20 at 40cm, and 0.73 or about 20/30 at 30cm. The combination also delivered binocular uncorrected distance visual acuity of 1.1 or a little better than 20/20 (Villegas EA et al. AJO 2014;157(1):142-149).
The trade-off is slightly worse distance vision in the non-dominant eye, and less near vison than a multifocal. Also, patients vary in their tolerance of spherical aberration, said Pablo Artal PhD, of the University of Murcia, Spain. However, using adaptive optics to determine the best combination of spherical aberration and defocus (sphere) correction for a given patient, the LAL allows for a truly customised solution, he added.
POLYFOCALITY
The WIOL-CF (Medicem) is a hydrogel lens 9.0mm in diameter with no haptics designed to fill the capsular bag and mimic the shape and function of the natural crystalline lens. It incorporates continuous aspheric hyperboloid polyfocal optic with higher power at the centre designed to provide up to 2.0D of continuous pseudo-accommodation, and may deform under accommodative effort to provide additional add power.
The trade-off is less near vision than a multifocal. In a study conducted by Dr Pallikaris, 72 per cent of patients achieved J2 or better near vision with 20/20 distance. Other studies have found uncorrected near vision of J3. Photopic and mesopic contrast sensitivity is within normal range. The lens also provides good stereopsis. Ray tracing shows a depth of focus of five to six dioptres at the lens centre, though in a very narrow zone. Dr Pallikaris expected a high myopic shift in the bright Greek sun, but patients notice it much less than he suspected. “It mimics somehow natural pseudo-accommodation that is quite acceptable to the patient,” he said.
Dr Pallikaris inserts the lens through a 2.8mm incision in a dehydrated state. The lens hydrates to fill the capsular bag in the first 48 hours.
While the various EDOF lenses are less prone to photic phenomena and provide continuous defocus, multifocals still provide better near vision, Dr Ang noted. “The EDOF lenses are here to stay but you cannot do away with the multifocal.”
In the end, patient needs drive the decision.
Ioannis G Pallikaris: pallikaris@dunyagoz.com
Oliver Findl: oliver@findl.at
Jorge L Alió: jlalio@vissum.com
Joseph JK Ma: joseph.ma@utoronto.ca
Robert Edward Ang: rtang@asianeyeinstitute.com
Pablo Artal: Pablo@um.es
Authors
Howard Larkin
Published
Wednesday, January 10, 2018
Category