Co-existing cataract and glaucoma
Soosan Jacob MD reports on the general principles of cataract and glaucoma and the basics of trabeculectomy
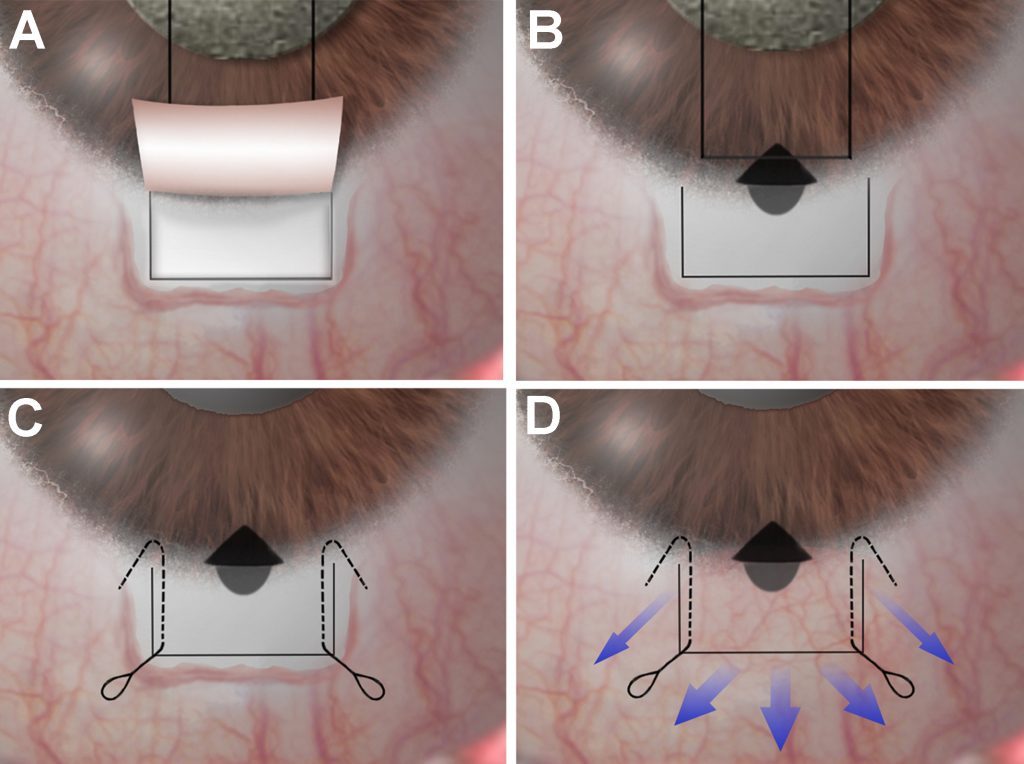 A- Conjunctival peritomy and scleral flap are followed by application of MMC; B- Sclerostomy and PI are done; C- Sutures are applied (conventional/ releasable/ adjustable); D- A posteriorly directed flow and diffuse bleb are attained
A- Conjunctival peritomy and scleral flap are followed by application of MMC; B- Sclerostomy and PI are done; C- Sutures are applied (conventional/ releasable/ adjustable); D- A posteriorly directed flow and diffuse bleb are attainedCataract and glaucoma may co-exist in the same patient and management depends on various factors, aims being effective IOP control and safety. Surgery is decided based on grade of cataract, severity of glaucoma, cause for decreased vision and target intraocular pressure (IOP).
A great deal of variation exists in choice of management among different surgeons. Part 1 of this multi-part article deals with general principles as well as the trabeculectomy technique. Subsequent parts will deal with other glaucoma surgeries.
CATARACT SURGERY ALONE
The patient should be assessed to know if visual loss is due to glaucoma, cataract or both. Very dense cataracts interfere with accurate glaucoma assessment. Though improvement on potential acuity meter helps rule out macular involvement, advanced field loss is not detected until fixation is involved. Early cataract affects visual quality more in patients with glaucoma and cataract extraction may be of benefit.
Conjunctival incisions should be avoided to maximise virgin conjunctiva and clear corneal phacoemulsification is preferred. Cataract surgery alone may decrease IOP slightly, with reduction being greatest in those with higher preoperative values. The “cataract alone” approach avoids risks of glaucoma surgery such as hypotonic maculopathy, shallow anterior chamber (AC), infection etc, especially in eyes with mild, medically well controlled glaucoma on single/ double drug. Close follow-up is required to assess the need for glaucoma surgery later.
Minimally invasive glaucoma surgery (MIGS) may be more safely combined in these patients as cataract surgery alone may not control IOP and sometimes may even result in loss of control. Cataract surgery carries higher risk with small pupil, rock hard cataracts, high myopia, pseudoexfoliation etc. and any ensuing vitreous loss can decrease success rate for subsequent glaucoma surgery. Angle closure may occur secondary to increasing size of the lens with age and can be treated effectively with phacoemulsification.
Risk of fixation loss following postoperative IOP spike in patients with advanced glaucoma should be kept in mind and should be strictly avoided by good surgical technique as well as with the use of beta blockers and carbonic anhydrase inhibitors. Retained viscoelastic, postoperative inflammation and steroid usage are risk factors.
GLAUCOMA SURGERY ALONE
This may be opted for in eyes with uncontrolled glaucoma despite maximum medical therapy/ laser trabeculoplasty. Surgical options include trabeculectomy, non-penetrating surgeries, glaucoma drainage devices and in mild cases, MIGS. However, cataract formation may be hastened and loss of IOP control is possible following subsequent cataract surgery resulting in need for further medical or surgical management.
Initial glaucoma surgery should therefore aim at lower target pressure so that subsequent cataract extraction still retains IOP within an acceptable range. Postoperative inflammation should be avoided after cataract surgery to prevent decrease in bleb function.
COMBINED SURGERY
Combined surgery is more convenient to the patient and can give better results with lesser need for medications as compared to cataract surgery alone. Though older studies indicate trabeculectomy has a greater IOP reduction than combined surgery, subsequent cataract surgery may result in loss of this beneficial effect.
Phacotrabeculectomy has been shown to have an equal pressure-lowering effect when used in conjunction with mitomycin C (MMC) but lesser when used with 5-fluorouracil. Antimetabolites can increase success rate but may be associated with complications such as thin, avascular leaking bleb, overfiltration, shallow AC, overhanging bleb, scleral melt, blebitis and endophthalmtis and should be used only as recommended.
Combined surgery avoids postoperative pressure spikes in advanced cases; however, this may still occur, especially with retained viscoelastic, blood/ fibrin in AC or tight flap sutures. Choice of glaucoma surgery depends on the stage of glaucoma. Trabeculectomy is the most commonly performed glaucoma filtration surgery worldwide and can be combined with phacoemulsification. Two-site surgery is more effective and safer than single-site.
Trabeculectomy: This may be opted for in medically uncontrolled patients. The Moorfields Safer Surgery System gives guidelines for effective IOP control while minimising complications and failure. Surgery is preferred in the superior quadrant to allow mechanical protection of the bleb by the upper lid, to decrease risk of inflammation and blebitis as well as to avoid diplopia with an exposed peripheral iridectomy (PI).
A 6-8mm peritomy with about a 10-15mm posterior dissection to all sides gives a fornix-based conjunctival flap and avoids the ‘ring of steel’ scarring as well as cystic bleb formation associated with limbus-based conjunctival flaps. This, together with stopping side cuts of a 3.5x4.5mm half thickness scleral flap short of the limbus, allows a diffuse, posteriorly filtering bleb. Gentle, focal cautery to arrest bleeding and avoiding creating the flap over large perforating aqueous veins is important.
Lamellar dissection is done just into the clear cornea and an antimetabolite is applied under the scleral and conjunctival flaps before entering the eye. MMC (0.2-0.5mg/ml, concentration depending on risk factors) is applied for two-to-three minutes over a large area, avoiding contact with conjunctival wound edges, followed by a thorough wash. An inferotemporal paracentesis or needle entry is made for forming the AC when required and an AC maintainer may be used.
When combined with phaco, the phaco ports are placed so as not to intersect the scleral flap. Side port may be used later for placing AC maintainer. After phaco and IOL implantation, a sclerostomy is made using blade and scissors or with single punch using 0.5mm Descemet membrane punch. The PI is made holding the scissor parallel to limbus to get an iridectomy that covers the extent of the sclerostomy. PI is avoided by some to decrease risk of postoperative inflammation/ hyphema and subsequent postoperative IOP spike/ bleb fibrosis. However, this is at the cost of an increased risk of iris adhering to and occluding the ostium.
Preplaced 10-0 nylon sutures at the flap corners are then tied and aqueous flow on irrigation as well as stability of AC on stopping irrigation act as a guide to the tightness of sutures as well as need for more sutures. The use of releasable and adjustable scleral flap sutures allows the ability to increase flow postoperatively.
A nylon suture on a round-bodied needle is finally used to apply continuous sutures to close the conjunctiva and phaco ports are checked for any leak. AC is formed again after removing speculum.
Dr Soosan Jacob is Director and Chief of Dr Agarwal's Refractive and Cornea Foundation at Dr Agarwal's Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
Authors
Soosan Jacob
Published
Monday, July 22, 2019
Category
Glaucoma
Tags