SMILE complications
Most challenges can be managed without affecting final visual outcome

Howard Larkin
Published: Saturday, June 1, 2019
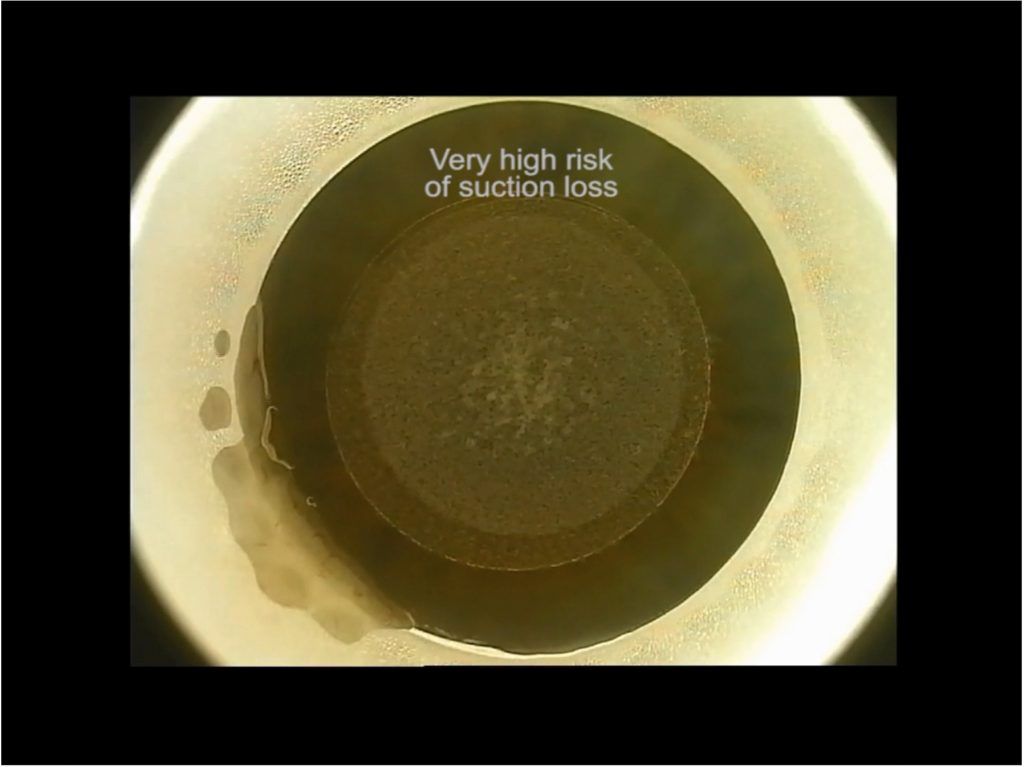 High risk of suction loss during the laser lenticule dissection due to fluid and conjunctival sliding into the contact glass/cornea interface. Image courtesy of Mario Nubile MD
With more than one million small-incision lenticule extraction (SMILE®) refractive procedures performed worldwide, a profile of the most common complications has emerged. Lenticule extraction difficulties and minor tears at the lenticule incision edge are among the more common complications specific to SMILE. The overall incidence of complications that may affect visual acuity after SMILE is very low and comparable to that of LASIK/PRK, according to literature review.
If well managed, most SMILE complications do not affect the final visual outcome, Mario Nubile MD told the International Society of Refractive Surgery Refractive Subspecialty Day at the American Academy of Ophthalmology 2018 Annual Meeting in Chicago, USA. He reviewed how to prevent and recover from some common SMILE problems.
Suction loss
Performed with a femtosecond laser docked to the cornea with a suction device, suction loss is more common in SMILE than femto-LASIK for two reasons, said Dr Nubile, of the University G. d'Annunzio, Chieti-Pescara, Italy. First, the SMILE cut takes longer, about 25-to-35 seconds. Second, the VisuMax® device uses a low-suction pressure to avoid injury. Suction loss risk factors include conjunctival chemosis, higher cylinder, narrow eyelids, smaller corneal diameter and lid squeezing and is more common in the early learning curve, though suction loss can occur at any time with any surgeon. Average incidence of suction loss reported in the literature ranges between 0.5 and 2%, but it decreases with surgeons’ experience.
In cases of suction loss during the side, anterior lenticule plane or first 10% of the posterior surface plane cut, the procedure can usually be recovered by carefully redocking the patient and restarting the procedure, Dr Nubile said. However, if lost after more than 10% of the posterior plane is cut, redocking will usually lead to aberrations near the corneal centre. In these cases, the SMILE procedure must be abandoned, though conversion to PRK or femto-LASIK is possible.
Opaque bubble layer
When bubbles from laser photo-disruption fail to dissipate, they can form an opaque layer that makes it impossible to visualise and perform lenticule dissection. The problem is usually associated with thin lenticules and thicker corneas, and can be minimised through optimal energy settings, Dr Nubile said. The solution is to wait for the bubbles to disappear. This may be accelerated by gently massaging them out from the lenticule interface. Opaque bubble layer formation generally does not affect visual outcomes.
Black spots
Adherence of water droplets or meibomian secretions on the interface between the suction cone and cornea can locally block photo-disruption, resulting in regional absence of tissue cleavage that appear as black spots on the cornea. These adhesions must be manually separated during lenticule dissection. However, this must be done carefully as it creates a risk of difficult extraction, incision tears and false dissection planes, Dr Nubile noted.
Incisional tear, cap perforation and false plane creation
These usually occur when instruments face tissue resistance during lenticule dissection, Dr Nubile said. The overall incidence of incisional tear is 1.8%, cap perforation 0.22% and false plane less than 0.2%. Tears and perforations usually are minor and can be managed with topical antibiotic gels and artificial tears, and usually do not permanently affect vision.
However, false plane creation can cause the lenticule to stack, making extraction difficult and risking incomplete lenticule removal, resulting in irregular astigmatism. This can be treated with topography-guided custom ablation, though corneal haze may result. False planes in the stroma under the posterior plane can lead to opacities and permanent haze. Specialised blunt dissection instruments can help prevent these complications.
Ectasia
While just seven cases of ectasia after SMILE have been reported, of which four had form fruste keratoconus, ectasia is a risk. For now, patients should be subject to the same screening requirements as for LASIK, including residual stromal bed and corneal thickness to reduce risks, Dr Nubile said.
Greater care should be taken during the SMILE learning phase, when most complications occur, Dr Nubile concluded.
“SMILE is quite a difficult surgery; it is not like a PRK and skill is required to avoid complications.”
High risk of suction loss during the laser lenticule dissection due to fluid and conjunctival sliding into the contact glass/cornea interface. Image courtesy of Mario Nubile MD
With more than one million small-incision lenticule extraction (SMILE®) refractive procedures performed worldwide, a profile of the most common complications has emerged. Lenticule extraction difficulties and minor tears at the lenticule incision edge are among the more common complications specific to SMILE. The overall incidence of complications that may affect visual acuity after SMILE is very low and comparable to that of LASIK/PRK, according to literature review.
If well managed, most SMILE complications do not affect the final visual outcome, Mario Nubile MD told the International Society of Refractive Surgery Refractive Subspecialty Day at the American Academy of Ophthalmology 2018 Annual Meeting in Chicago, USA. He reviewed how to prevent and recover from some common SMILE problems.
Suction loss
Performed with a femtosecond laser docked to the cornea with a suction device, suction loss is more common in SMILE than femto-LASIK for two reasons, said Dr Nubile, of the University G. d'Annunzio, Chieti-Pescara, Italy. First, the SMILE cut takes longer, about 25-to-35 seconds. Second, the VisuMax® device uses a low-suction pressure to avoid injury. Suction loss risk factors include conjunctival chemosis, higher cylinder, narrow eyelids, smaller corneal diameter and lid squeezing and is more common in the early learning curve, though suction loss can occur at any time with any surgeon. Average incidence of suction loss reported in the literature ranges between 0.5 and 2%, but it decreases with surgeons’ experience.
In cases of suction loss during the side, anterior lenticule plane or first 10% of the posterior surface plane cut, the procedure can usually be recovered by carefully redocking the patient and restarting the procedure, Dr Nubile said. However, if lost after more than 10% of the posterior plane is cut, redocking will usually lead to aberrations near the corneal centre. In these cases, the SMILE procedure must be abandoned, though conversion to PRK or femto-LASIK is possible.
Opaque bubble layer
When bubbles from laser photo-disruption fail to dissipate, they can form an opaque layer that makes it impossible to visualise and perform lenticule dissection. The problem is usually associated with thin lenticules and thicker corneas, and can be minimised through optimal energy settings, Dr Nubile said. The solution is to wait for the bubbles to disappear. This may be accelerated by gently massaging them out from the lenticule interface. Opaque bubble layer formation generally does not affect visual outcomes.
Black spots
Adherence of water droplets or meibomian secretions on the interface between the suction cone and cornea can locally block photo-disruption, resulting in regional absence of tissue cleavage that appear as black spots on the cornea. These adhesions must be manually separated during lenticule dissection. However, this must be done carefully as it creates a risk of difficult extraction, incision tears and false dissection planes, Dr Nubile noted.
Incisional tear, cap perforation and false plane creation
These usually occur when instruments face tissue resistance during lenticule dissection, Dr Nubile said. The overall incidence of incisional tear is 1.8%, cap perforation 0.22% and false plane less than 0.2%. Tears and perforations usually are minor and can be managed with topical antibiotic gels and artificial tears, and usually do not permanently affect vision.
However, false plane creation can cause the lenticule to stack, making extraction difficult and risking incomplete lenticule removal, resulting in irregular astigmatism. This can be treated with topography-guided custom ablation, though corneal haze may result. False planes in the stroma under the posterior plane can lead to opacities and permanent haze. Specialised blunt dissection instruments can help prevent these complications.
Ectasia
While just seven cases of ectasia after SMILE have been reported, of which four had form fruste keratoconus, ectasia is a risk. For now, patients should be subject to the same screening requirements as for LASIK, including residual stromal bed and corneal thickness to reduce risks, Dr Nubile said.
Greater care should be taken during the SMILE learning phase, when most complications occur, Dr Nubile concluded.
“SMILE is quite a difficult surgery; it is not like a PRK and skill is required to avoid complications.”