Sensing Improved Phaco Safety
Handpiece with dynamic IOP sensor protects against occlusion surge. Dermot McGrath reports

Howard Larkin
Published: Tuesday, August 31, 2021
A new phacoemulsification handpiece that includes an integrated pressure sensor may help overcome problems associated with variable infusion and aspiration rates that affect intraocular pressure (IOP) during cataract surgery, according to a study presented at the online annual meeting of the French Implant and Refractive Surgery Association (SAFIR).
“This handpiece allows us to operate closer to the real-time physiological IOP of the patient. It also protects against post-occlusion surges and incision leaks and provides automatic detection of the patient eye level (PEL), which is important to calibrate the fluidics accurately in the system,” said Pascal Rozot MD, Clinique Juge, Marseille, France.
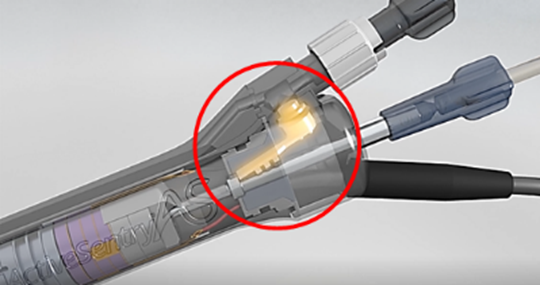
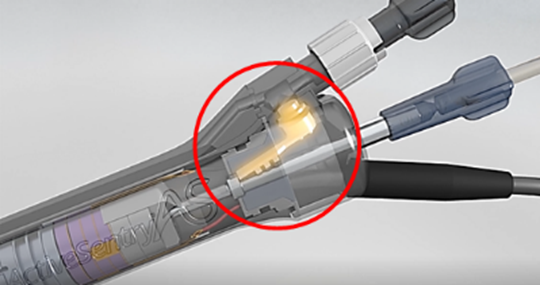
With the traditional handpiece, pressure alterations at the phaco probe tip travelled to a sensor near the cassette at the speed of sound with adjustments made at the Active Fluidics unit level. Using the ACTIVE SENTRY handpiece, however, the IOP is measured in real-time, intraoperatively, as the new handpiece is equipped with an integrated pressure sensor (Fig 1) and communicates directly with the fluidics regulation system. The result is a faster response to fluctuations in IOP during surgery and greater anterior chamber stability, Dr Rozot explained.
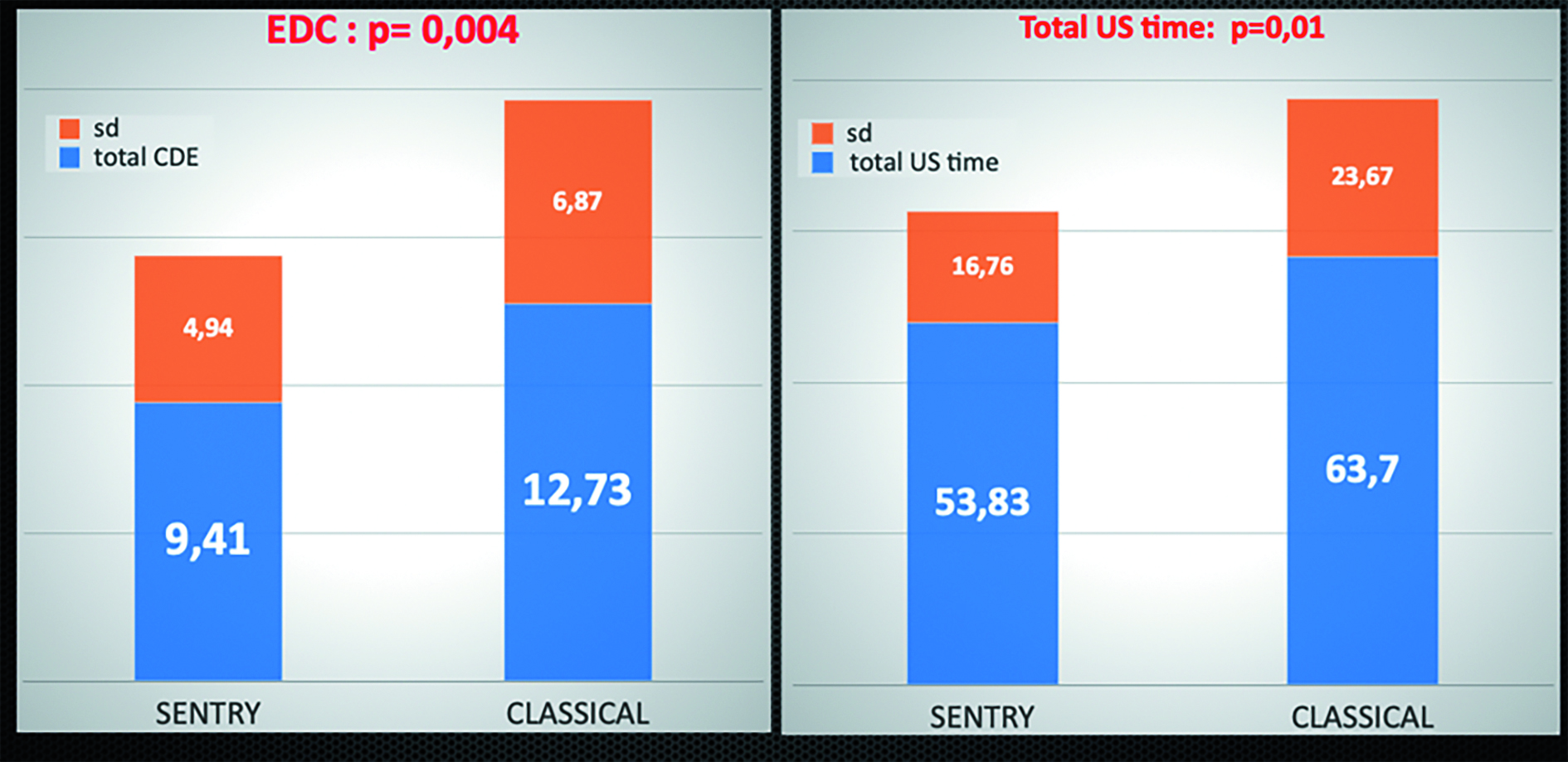
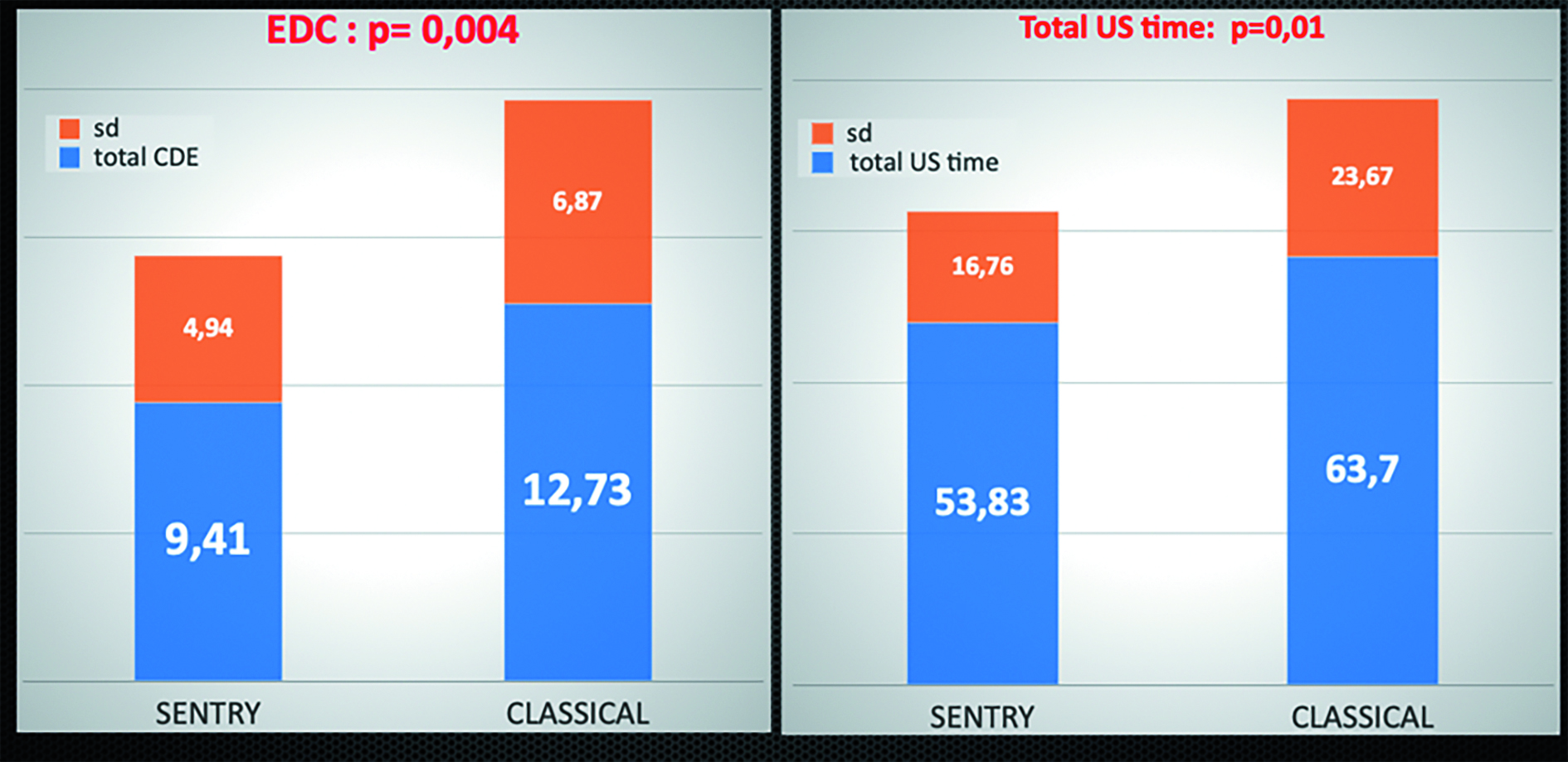
Dr Rozot’s prospective non-randomised study compared the performance of the new ACTIVE SENTRY handpiece (Alcon Laboratories) to the classic handpiece on the Centurion Vision System (Alcon). A total of 109 eyes were included and divided into two groups matched for age, sex, and cataract density: 43 eyes for ACTIVE SENTRY and 66 eyes for the classic handpiece. Due to the higher performance of the ACTIVE SENTRY handpiece, aspiration parameters used for the quadrants’ nucleus removal increased by 25%, whereas the IOP could lower to 34mmHg. The parameters assessed included total intervention time, cumulative dissipated energy (CDE), total ultrasound time, fluid use, and total aspiration time.
In terms of outcomes, the total intervention time was slightly longer for the ACTIVE SENTRY handpiece group, but the difference was not statistically significant. The total CDE significantly reduced using the ACTIVE SENTRY handpiece (9.41 seconds) compared to the classic handpiece (12.73 seconds). Total ultrasound time was also reduced from a mean of 63.7 with the classic handpiece to 53.8 with ACTIVE SENTRY (Fig 2). Fluidics use reduced, too, with ACTIVE SENTRY (43.35 cc) compared to the traditional handpiece (47.26 cc).
Putting the results into context, Dr Rozot said less energy delivered into the eye with ACTIVE SENTRY should equate to safer, more stable surgery.
“ACTIVE SENTRY reduced the quantity of fluid used by around 8% with a reduction of up to 25% ultrasound energy delivered into the eye. The new handpiece enables us to work with a physiological IOP and protect against occlusion surge. I think it will be particularly valuable to use in high-risk cases such as high myopes, loose zonules, and floppy iris syndrome where greater anterior chamber stability is required,” he concluded.
Pascal Rozot: pascal.rozot@dr-rozot.com
Declaration of interest: Consultant for Alcon, Johnson & Johnson, Carl Zeiss Meditec, Thea
Tags: retina
Latest Articles
Beyond the Numbers
Empowering patient participation fosters continuous innovation in cataract surgery.
Thinking Beyond the Surgery Room
Practice management workshop focuses on financial operations and AI business applications.
Picture This: Photo Contest Winners
ESCRS 2025 Refractive and Cataract Photo Contest winners.
Aid Cuts Threaten Global Eye Care Progress
USAID closure leads retreat in development assistance.
Supplement: ESCRS Clinical Trends Series: Presbyopia
Nutrition and the Eye: A Recipe for Success
A look at the evidence for tasty ways of lowering risks and improving ocular health.
New Award to Encourage Research into Sustainable Practices
Sharing a Vision for the Future
ESCRS leaders update Trieste conference on ESCRS initiatives.
Extending Depth of Satisfaction
The ESCRS Eye Journal Club discuss a new study reviewing the causes and management of dissatisfaction after implantation of an EDOF IOL.
Conventional Versus Laser-Assisted Cataract Surgery
Evidence favours conventional technique in most cases.