Positive results experienced with surgery that addresses underlying nerve loss.
Cheryl Guttman Krader reports.
While there are multiple supportive surgical and nonsurgical treatments for neurotrophic keratopathy, corneal neurotisation is the only intervention addressing the underlying loss of corneal innervation and has shown corneal sensation improvement in humans, according to Ilya M Leyngold MD.
“Corneal neurotisation reinnervates the cornea through the transfer of an intact donor sensory nerve. It thereby re-establishes lost or impaired corneal sensation and supportive trophic functions, leading to restoration of corneal integrity,” Dr Leyngold said.
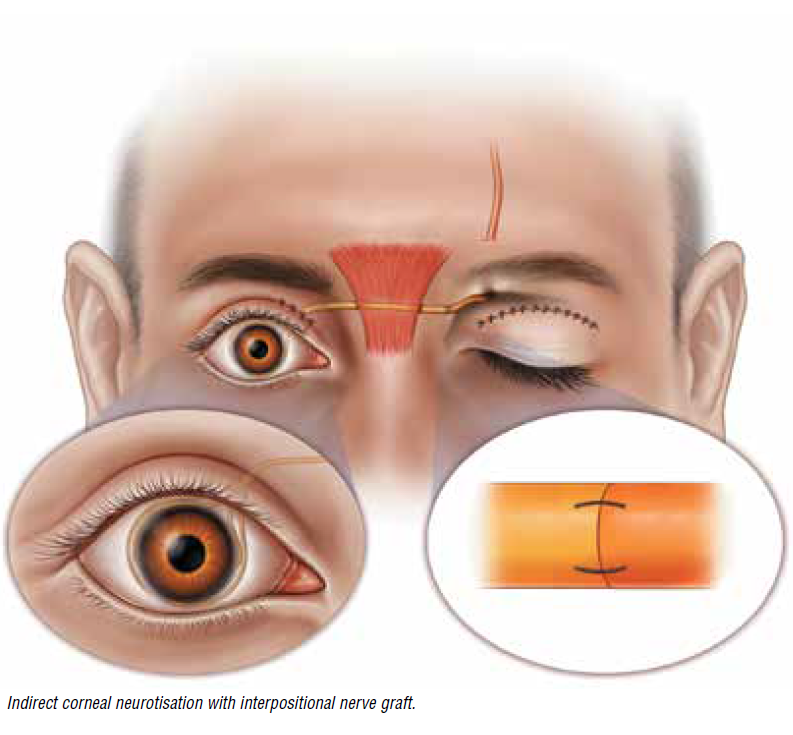
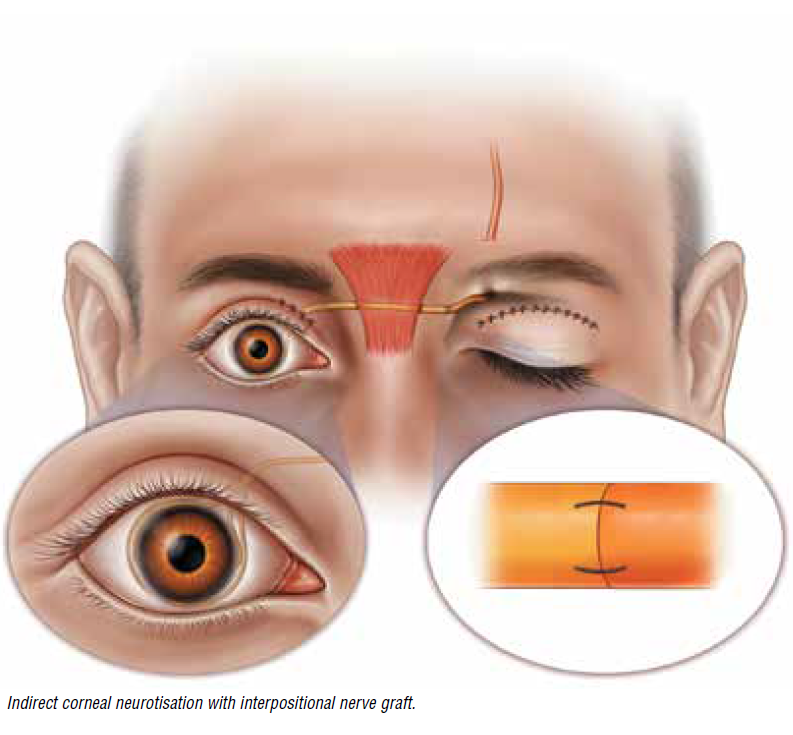
First described in the peer-reviewed literature in 2009, corneal neurotisation is a relatively new procedure. But already, several technique modifications have been introduced that use different nerve sources and transfer approaches. The technique used in the first published report involved extensive facial dissection with contralateral supraorbital nerve and supratrochlear nerve harvesting through a coronal incision and tunnelling the nerves across the bridge of the nose to the limbus for direct neurotisation. Subsequently, various groups developed minimally invasive approaches for performing direct corneal neurotisation that used palpebral or sub-brow incisions for harvesting and transferring the donor nerve, including Dr Leyngold and colleagues.
Indirect corneal neurotisation with an interpositional nerve autograft was first reported in 2014 literature by Canadian surgeons who used a sural nerve autograft coapted to the supratrochlear nerve. Others have performed the indirect transfer using other nerves for the autograft. As first reported by Dr Leyngold and colleagues, the indirect transfer approach has also been performed using processed nerve allograft to eliminate the need for donor harvesting.
“There are multiple factors to consider when deciding on the surgical approach for corneal neurotisation. There are also questions that remain—including which is better, direct or indirect transfer, or allograft versus autograft; what is the effect on the outcome with the use of nerve growth factors; and how should the fascicles be positioned around the cornea,” he noted.
SURGICAL SUCCESS
Dr Leyngold discussed outcomes after corneal neurotisation by reviewing a recently published study that he co-authored.i The research analysed data from 24 eyes of 23 patients having a minimum follow-up of six months after minimally invasive direct corneal neurotisation or indirect corneal neurotisation using processed nerve allograft.
Among 13 eyes that presented with a persistent epithelial defect, 11 eyes (85%) achieved complete closure maintained at the last available follow-up. In the total series, 23 eyes (92%) had improvement in ocular surface quality. Cochet-Bonnet aesthesiometry measurements of corneal sensation showed a median gain of 2.3 cm. Most of the improvement in aesthesiometry measurements occurred within the first six months, but individual responses varied. Partial or full return of skin sensation around the donor site was reported by 94% of patients who provided self-assessment. Mean visual acuity did not change significantly after surgery.
“Patients must be counselled that corneal neurotisation does not result in overnight success. Improvements usually occur in 6 to 12 months, but it can take two or three years. In addition, the surgery does not necessarily result in visual improvement because patients may have scarring or other comorbid ocular conditions that limit visual potential,” Dr Leyngold emphasised.
“However, corneal neurotisation can allow for other procedures, such as corneal transplantation, that will restore vision. And in our study, all 17 patients who provided a self assessment of their outcome said they would go through the surgery again if they had the choice.”
PRACTICAL PEARLS
Dr Leyngold presented a schematic of his current algorithm for deciding on the corneal neurotisation approach that takes into account the availability of a donor nerve with sensory function and the aetiology of the neurotrophic keratopathy. Other issues considered when choosing candidates for the surgery include previous treatments tried and local or systemic factors that can affect the surgery or its outcome, such as the conjunctiva’s condition and whether the patient is currently undergoing local radiation or chemotherapy.
Considering the risk of amblyopia, Dr Leyngold said he tends to be more aggressive performing the surgery sooner versus later in paediatric patients.
For surgeons interested in performing corneal neurotisation, Dr Leyngold suggested using a team approach that either combines the expertise of corneal and oculoplastic surgeons or includes physicians who specialise in otolaryngology or plastic surgery. For greater technical ease, he advised choosing patients who have an available ipsilateral donor nerve to help avoid the need to do cross-face transfer of a contralateral nerve and starting with patients who do not have conjunctival scarring, which makes dissection more complicated.
“Preferably also start with healthier patients because they tend to have better outcomes,” he added.
This presentation was made at AAO 2021 in New Orleans, Louisiana, USA.
i Rafailov L, et al. Cornea. 2021; 40: 1377–1386.
Ilya M Leyngold MD is an oculofacial plastic surgeon at the Leyngold Institute for Plastic Surgery, Meridian, Idaho, USA.
ileyngo1@gmail.com