Cataract, Refractive
Latest ESCRS Clinical Trends Survey
This current ESCRS survey reports on trends in our field over time and demonstrates nicely how our subspecialty continues to change.

Presbyopia IOL use steady, but obstacles remain. Cost to the patient, concerns over contrast visual acuity, and night-time quality of vision are the main reasons cited for not performing more presbyopia IOL procedures, suggest the data from the latest ESCRS Clinical Trends Survey.
Professor Rudy MMA Nuijts, University Eye Clinic Maastricht, Netherlands, presented the latest survey results at an ESCRS IME symposium on the opening day of the ESCRS Winter Meeting in Vilamoura, Portugal.
More than 1,700 delegates responded to 146 survey questions during the 40th ESCRS Annual Congress Milan, the eighth year this survey was conducted.
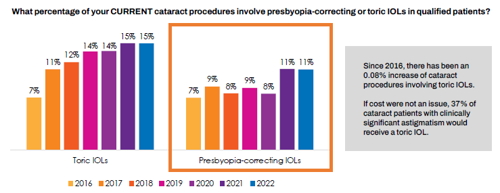
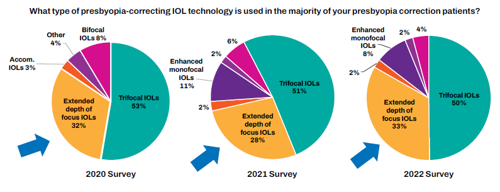
Eleven percent of respondents were implanting presbyopia- correcting IOLs, the same percentage as the previous year. Similarly, trifocal IOLs accounted for the same percentage as the previous year, 50% of cases. Extended depth of focus IOLs saw a small increase to 33% from 28%. Accommodating and bifocal IOLs were used in 2% and 4% of cases, respectively.
Regarding their biggest concerns about performing more presbyopia-correcting IOL procedures, members cited cost to patient, concerns over contrast visual acuity, and night-time quality of vision. Twenty percent also expressed concerns about inadequate unaided near-vision results.
Since 2016 there has been an 8% increase in cataract procedures using toric IOLs. The survey showed no clear consensus on the best approach in cases where the cylinder was 1.25 D or less, with many surgeons preferring on-axis incisions. However, toric IOLS were the clear favourite in cases of astigmatism of at least 1.75 D.
Cost remains the leading concern limiting the use of toric IOLs. If cost were not an issue, 37% of cataract patients with clinically significant astigmatism would receive a toric IOL, Prof Nuijts noted.
The survey comes on the heels of a JCRS review of data gleaned from the previous ESCRS surveys.1 “This current ESCRS survey reports on trends in our field over time and demonstrates nicely how our subspecialty continues to change,” said Professor Thomas Kohnen in an accompanying editorial. “Research in cataract and refractive surgery keeps moving us forward to evolve our practices for the benefit of our patients.”
Postoperative success with toric IOLs, he added, is dependent on placement accuracy and rotational stability: “The introduction of digital image guidance systems has improved the former; however, the latter varies across different toric IOL models, and ASCRS and ESCRS delegates are variably stringent with acceptable thresholds of postoperative rotational error,” he said. “Comparing ESCRS and ASCRS respondents, 16.0% and 9.4% are comfortable with ≥10 degrees, compared with >65.0% and 53.8%, respectively, agreeing visual quality and acuity would be significantly affected by ≥5 degrees of rotational error.
“Surveys such as these are important tools to evaluate how real-world practice patterns align with recommended evidence-based standards of care and highlight areas where patient care can be enhanced through the adoption of new technologies and/or surgical approaches.”
For citation notes, see page 46.
The ninth ESCRS Clinical Trends Survey will be conducted in September 2023 at the ESCRS Annual Congress in Vienna.
Rudy MMA Nuijts MD, PhD is professor of ophthalmology, vice-chairman, and director of the Cornea Clinic and the Center for Refractive Surgery at the University Eye Clinic Maastricht, Netherlands.
Thomas Kohnen MD, PhD, FEBO is professor and chair, Department of Ophthalmology, Goethe University, Frankfurt, Germany.