Cataract, IOL, EURETINA
Surgery for IOL Luxation in Vitrectomised Eyes
Decision making requires consideration of numerous factors.

Cheryl Guttman Krader
Published: Wednesday, January 7, 2026
“ Late IOL luxations are becoming more frequent, probably due to longer life expectancy and increasing numbers of younger people undergoing phacorefractive surgery. “
Multiple options exist for managing intraocular lens (IOL) luxation in a vitrectomised eye. With a surgical plan that considers the pros and cons of the various choices, the existing clinical situation, and surgeon expertise, a good and stable refractive outcome can be achieved in most cases, said Silvia Bopp MD.
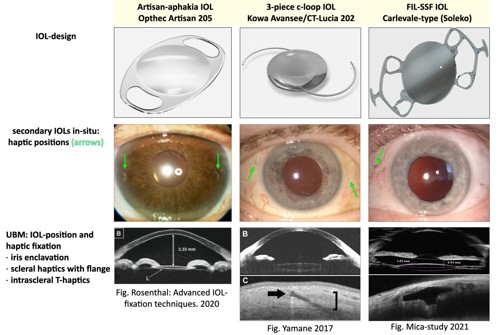
Speaking during a EURETINA/ESCRS joint symposium in Paris, Dr Bopp discussed considerations for choosing refixation versus IOL exchange. In addition, she reviewed IOL choices and fixation techniques with a focus on the advantages, limitations, and indications for using the iris-fixated Artisan Aphakia lens (model 205), scleral-fixated three-piece foldable hydrophobic acrylic IOLs with polyvinylidene fluoride (PVDF) haptics (e.g., Avansee, Kowa and CT Lucia 202, Zeiss), and the FIL-SSF (foldable intraocular lens – sutureless scleral fixation, Carlevale) IOL as secondary implants.
Based on these issues, Dr Bopp said her preference is to perform an IOL exchange using the FIL-SSF IOL.
“The FIL-SSF is the only IOL that has been specifically developed and approved for scleral fixation,” she explained. “It is a foldable lens with a large (6.5 mm) optic, and the implantation surgery, which is a sutureless technique, is a reproducible procedure. In addition, because of its specific design that provides four-point support with two-point fixation, the FIL-SSF IOL maintains a stable position postoperatively. In fact, studies show the degree of postoperative tilt with the FIL-SSF IOL is comparable to that of IOLs implanted in an intact capsular bag.”
Pros and cons of refixation
Dr Bopp said the main advantage of reusing the primary IOL is that, compared to an exchange procedure, the surgery itself exposes the cornea to less iatrogenic stress. When considering refixation, however, surgeons need to think about the exact design of the primary IOL in terms of its shape, dimensions, and angulation.
“My recommendations are that a three-piece hydrophobic IOL with filamentous (flexible) haptics are best suited for reimplantation and that they should be refixated with a sutureless technique,” Dr Bopp said.
She advised against refixation of one-piece IOLs because these implants usually have sharp edges and no angulation. Therefore, their repositioning risks the development of reverse pupillary block and uveitis/glaucoma/hyphaema.
In addition, the suturing technique can be challenging, and with the two-point fixation, it can be difficult to achieve a truly tilt-free, symmetric position.

Options for IOL exchange
Discussing the Artisan Aphakia, three-piece foldable hydrophobic acrylic IOLs, and FIL-SSF IOL as options for exchange, Dr Bopp said the advantages of the Artisan IOL include its use with or without anterior or complete vitrectomy, its fast and easy implantation, and its ability to provide a good barrier if gas or silicone tamponade is needed. However, the Artisan IOL also has several drawbacks, including a relatively small optic (5.0 mm), its rigid PMMA material that mandates implantation through a 5.0 mm incision, and risks for inducing iridodonesis, pupil distortion, and uveitis. It also carries a 5% risk of chronic cystoid macular oedema and a 10% rate of haptic release.
“The indication for using an Artisan IOL would be a healthy eye with a robust, pigmented iris and no uveitis, glaucoma, or retinal detachment,” Dr Bopp said, adding that outcomes for achieving a target refraction within 1.0 D and for maintaining positional stability are poorer for the Artisan IOL compared with the FIL-SSF and three-piece IOLs.
The three-piece hydrophobic acrylic IOLs can be implanted with a sutureless scleral tunnel technique and are versatile and practically universally applicable. However, complete pars plana vitrectomy (PPV) is necessary when choosing one of these lenses, and there are postoperative risks of haptic externalisation as well as tilt and iris capture if the scleral tunnel is not perfectly symmetrical when created. Data on achieving target refraction and centration, tilt, and stability show outcomes with the three-piece IOLs are not as good as with the FIL-SSF, Dr Bopp said.
Complete PPV is also necessary when using the FIL-SSF IOL, and it carries a risk of reverse pupillary block. Additionally, its hydrophobic material means calcification can occur if there is a later need for air or gas tamponade.
“With the latter risk in mind, the FIL-SSF IOL should be used in patients with a stable retinal situation,” Dr Bopp said.
A looming epidemic
Dr Bopp observed that late IOL luxations are becoming more frequent, probably due to longer life expectancy and increasing numbers of younger people undergoing phacorefractive surgery.
“Considering that 50% of the population is 50 years and older and potential candidates for lens replacement, the cumulative incidence of IOL subluxation is 3% over 25 years,” she said. “As late IOL dislocation occurs at an average of 8 to 12 years, we can expect a wave for such problems.”
The likelihood of needing to manage IOL subluxation in a vitrectomised eye is increased by the fact that previous vitrectomy is a leading risk factor for this complication.
“In our clinic, about 60% of late IOL dislocations were in eyes with previous vitrectomy,” Dr Bopp said.
Dr Bopp spoke during a joint ESCRS/EURETINA symposium at EURETINA 2025 in Paris.
Silvia Bopp MD is a senior consultant specialising in retinal and vitreous surgery at Bergman Clinics, Bremen, Germany. silviabopp@icloud.com