Cornea
Six Essentials to Iris Repair
In the first of a multi-part series, Dr Soosan Jacob describes an introduction to the basics of iris repair.

Soosan Jacob
Published: Thursday, February 1, 2024
Iris repair is an integral part of many ocular surgeries, and every anterior segment eye surgeon should learn a few basic techniques. Usually performed as part of anterior segment reconstruction, it is sometimes also required of cataract surgeons, e.g., in case of iris damage following continual iris prolapse in intraoperative floppy iris syndrome. Complex surgeries that require peripheral anterior synechiolysis or release of posterior synechiae may also necessitate iridoplasty techniques.
In addition, sometimes one may need to operate on a patient with cataract co-existent with pre-existing iris damage—either as part of a pathology (e.g., iridocorneal endothelial syndrome) or secondary to post-traumatic/iatrogenic iris damage. In all these situations, it is beneficial to be wellversed in basic iris repair techniques. This multi-part series on iris repair will cover everything about the topic.
Iris anatomy
The iris consists of the pupillary and ciliary zones, with the thickest part the collarette (lying 2 mm around the pupil) and the thinnest the iris root. The circular sphincter pupillae and the radial dilator pupillae constrict and dilate the pupil, respectively. The pupillary ruff is the dark border of the pupil and formed by the posterior pigment epithelium wrapping around the pupillary margin. The anterior ciliary and long posterior ciliary arteries anastomose in the ciliary body (CB) to form the major and minor arterial circles that lie in the anterior part of the CB and along the pupillary border and are joined by radial vessels weaving through the iris stroma. The formed radial network can bleed into the anterior chamber (AC) during surgical iris trauma.
Synechiolysis
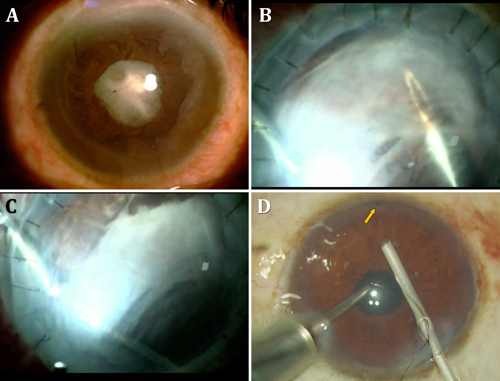
Peripheral anterior synechiolysis is sometimes needed in patients with prior surgery or other pathology. The iris should be carefully examined for signs of neovascularisation, atrophy, or prior defects. In every synechiolysis case, care should be taken to keep the AC pressurized, which may be done using viscoelastic or an AC maintainer and working through small incisions. Pressurization of the chamber is important to rapidly tamponade any possible bleeding from the iris. Hypotony will delay clotting and keep blood oozing for longer. Synechiolysis should be done gently by viscodissection, and if this proves difficult, then with either the rounded viscoelastic cannula or a blunt rod. Rough manoeuvres should be avoided as this can lead to iris tears, iridodialysis, and even Descemet’s detachment.
Posterior synechiolysis is required in some cases, especially post-uveitic cataracts. These can also often be released by gentle viscodissection. However, the pupil may remain non-dilating, and if additional procedures (such as cataract extraction, IOL explantation, or vitrectomy) are needed, some other pupillary dilatation technique such as mini-sphincterotomies, iris hooks, B-Hex, or Malyugin ring may be needed. Some of these cause iris tears and need iris repair, while others are gentler on the sphincter and do not need additional procedures.
Iridectomy
Though iridectomy is not a type of iris repair, it is sometimes required in combination with anterior segment reconstruction surgeries and often required during glaucoma, corneal, or vitreoretinal procedures. A peripheral iridectomy is best done in the superior periphery but may be required inferiorly to prevent a pupillary block when air or silicone oil is left in the eye. It may be done preoperatively using a YAG laser but also intraoperatively using a vitrector in I/A-cut mode with a very low cut rate and vacuum of about 300 mmHg. It is done after constricting the pupil using intracameral miotics.
In pseudophakic eyes, Fang et al. have described a technique of introducing a sharp needle (with its tip bent to 45 degrees) posterior to the iris that is bellowed upwards with viscoelastic.1 The bend is held horizontally to prevent iris snag and, once in position, turned anteriorly to engage the iris while applying posterior pressure with an iris repositor. The puncture is then enlarged with a microscissor. The approach should be from a comfortable angle for both instruments. Techniques that involve cutting the iris directly below the base of an incision run the risk of a poorly positioned iridectomy and iris base damage.
Iris membranes
The iris is a pro-inflammatory structure and iris membranes can often form, especially after severe episodes of intraocular inflammation. These membranes are fibrotic with varying levels of vascularisation and can hold the iris fixed in different positions. Membrane peeling can be done from over the iris using a combination of instruments. The sharp point of a 23-gauge needle can be inserted under the membrane, and the membrane gently dissected off the iris. Microforceps and microscissors can also be used to cut fibrous strands and remove them. Often, the entire iris then becomes mobile and free if not excised during any previous surgery. This freed iris tissue can then be pulled into position for iridoplasty.
Pupillary fibrous membrane
Sometimes a pupillary membrane may be found occluding the pupil, especially if associated with pre-existing uveitis, rubeosis, trauma, or post-surgical inflammation. This may be peeled off using microforceps or, if difficult, cut and removed using a combination of microforceps and microscissors or even a vitrector. In case of phakic eyes, care should be taken not to damage the lens. Sometimes, a fibrous band may encircle the pupillary aperture, and this can also be removed using microforceps.
Management of iris defects without intraocular surgery
Iris defects may exist from a previous surgery or trauma. This may result in photophobia, difficulty looking at light, polyopia, stray light, etc. Iris defects may be managed conservatively using tinted glasses or aniridic contact lenses, which have a clear central optic zone and a coloured periphery. Focal corneal tattoos may also be helpful in certain situations—e.g., if a peripheral iridectomy or an iridodialysis is not covered by the lid, causing symptoms. It can also be used for traumatic iris defects and aniridia. Tattoo application can be superficial or intra-lamellar into a femtosecond laser-created channel.
The next article in this series on iris repair will deal with pupilloplasty techniques. Stay tuned!
1. A Fang, et al., BMC Ophthalmology, 2018; 18(120).
Soosan Jacob MS, FRCS, DNB is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.
Update on Astigmatism Analysis
Is Frugal Innovation Possible in Ophthalmology?
Improving access through financially and environmentally sustainable innovation.
iNovation Innovators Den Boosts Eye Care Pioneers
New ideas and industry, colleague, and funding contacts among the benefits.
José Güell: Trends in Cornea Treatment
Endothelial damage, cellular treatments, human tissue, and infections are key concerns on the horizon.
Making IOLs a More Personal Choice
Surgeons may prefer some IOLs for their patients, but what about for themselves?
Need to Know: Higher-Order Aberrations and Polynomials
This first instalment in a tutorial series will discuss more on the measurement and clinical implications of HOAs.
Never Go In Blind
Novel ophthalmic block simulator promises higher rates of confidence and competence in trainees.