Cataract, Refractive, Retina, EURETINA
Retinal Detachment After Cataract Surgery
Knowledge of risk factors directs patient management and informed consent.

Cheryl Guttman Krader
Published: Wednesday, January 7, 2026
The incidence of rhegmatogenous retinal detachment (RRD) is increasing globally, and cataract/refractive lens surgery is a known risk factor for this event.
Speaking during a EURETINA/ESCRS joint symposium in Paris, Martin S Zinkernagel MD, PhD discussed risk factors for RRD after cataract surgery and risk mitigation strategies as a guide to appropriate patient counselling, preoperative intervention, and postoperative follow-up.
Who is at risk?
Findings from multiple studies identify male sex, high myopia, history of RRD in the fellow eye, absence of complete posterior vitreous detachment (PVD), and lattice degeneration as risk factors for RRD in general and/or after cataract surgery.1–4 In addition, a cohort analysis showed that among cases of pseudophakic RRD, the highest risk of RRD was in the 40- to 55-year-old age group.1“This information underscores a need to be particularly cautious about performing elective lens surgery in these young patients,” Dr Zinkernagel said.
The association between younger age and pseudophakic RRD risk corresponds with data showing that PVD prevalence increases with age. But while preoperative PVD is associated with a decreased risk of RRD after cataract surgery, its development after cataract surgery is certainly a major driver causing postoperative RRD.
“It is important to remember that 27% to 60% of eyes develop PVD within 1 year after cataract surgery.5 This rate of progression is much faster than in unoperated eyes,” Dr Zinkernagel said.
Risk mitigation
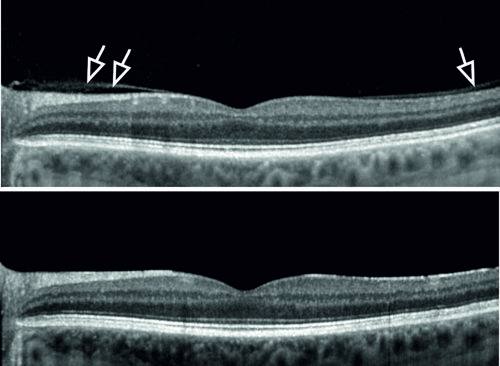
Determining vitreous and retina status preoperatively will help surgeons identify patients at risk for RRD after cataract surgery. Vitreous attachment is easily identified using optical coherence tomography (OCT), and Dr Zinkernagel mentioned that a project underway in his department aims to develop a deep learning-based screening system for automated detection of peripheral retinal breaks and detachments on fundus photography images.6
He advised that any existing retinal tears should be treated with laser before a patient undergoes cataract surgery, especially when there is no pigment or the lesion is a horseshoe tear rather than a round hole. The need to treat lattice degeneration is less clear.
“Even though lattice degeneration has been identified as an RRD risk factor, there is conflicting information about whether there is benefit for its prophylactic treatment,” Dr Zinkernagel said.
“Retinopexy is usually not recommended, but I [typically use] laser peripheral degenerations in eyes with significant risk factors for RRD, such as absence of PVD or a history of RRD in the fellow eye.”
Prompt recognition
The risk of RRD after cataract surgery is highest in the initial months and remains substantial during the first postoperative year but continues to be elevated for up to 10 years.1 Dr Zinkernagel recommended that patients at high risk for RRD after cataract surgery be monitored closely for several months postoperatively using multimodal imaging (OCT/widefield retina imaging) to identify development of PVD and retinal breaks. In addition, the informed consent for all patients undergoing cataract surgery should mention a reminder to watch for RRD warning signs (flashes, floaters, or shadows) and to seek care immediately if they occur. This information should be reinforced to high-risk patients.
Dr Zinkernagel presented during a joint ESCRS/EURETINA symposium at EURETINA 2025 in Paris.
Martin S Zinkernagel MD, PhD is Professor and Head of the Department of Ophthalmology at the University of Bern, Switzerland. martin.zinkernagel@insel.ch
1. Bjerrum SS, et al. Ophthalmology, 2013 Dec; 120(12): 2573–2579.
2. Hajari JN, et al. Retina, 2014 Aug; 34(8): 1658–1665.
3. Ludwig CA, et al. Sci Rep, 2023 Jun 9; 13(1): 9430.
4. Wallsh JO, et al. Ophthalmology, 2023 Jun; 130(6): 624–630.
5. Hayashi S, et al. Eye (Lond), 2022 Oct; 36(10): 1872–1877.
6. Christ M, et al. Transl Vis Sci Technol, 2024 Apr 2; 13(4): 1.