Cataract, Glaucoma
Harmonizing Eye Health
Cataract surgeons in the glaucoma symphony.

Howard Larkin
Published: Monday, October 2, 2023
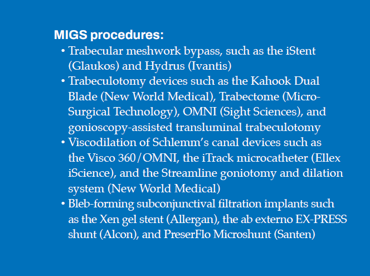
Over the past two decades, glaucoma treatments have proliferated with laser and less-invasive surgical options, filling in some of the gap between medical treatment for mild to moderate glaucoma and trabeculectomy to control advanced disease. As a result, ophthalmologists who mainly do cataract surgery now have glaucoma treatment options compatible with phacoemulsification, notably the various minimally invasive glaucoma surgery (MIGS) procedures.
 “The advent of MIGS signifies a change in glaucoma care for cataract surgeons,” Dr Roberto Bellucci said. Though his practice is primarily cataract and refractive surgery, having trained in a glaucoma clinic, he has done more than 2,000 glaucoma procedures—including trabeculectomies before filtering implants were available.
“The advent of MIGS signifies a change in glaucoma care for cataract surgeons,” Dr Roberto Bellucci said. Though his practice is primarily cataract and refractive surgery, having trained in a glaucoma clinic, he has done more than 2,000 glaucoma procedures—including trabeculectomies before filtering implants were available.
However, while glaucoma and cataract procedures use the same basic surgical skills, glaucoma surgery also typically requires intraoperative gonioscopy and detailed knowledge of angle anatomy.
In addition, glaucoma requires lifelong follow-up to detect and treat progression, which may not fit well with a streamlined cataract practice. Lack of reimbursement for more recent glaucoma devices and procedures, as well as the local out-of-pocket cost of eye drops, are other factors that may affect their uptake.
As a result, adding glaucoma treatment, especially surgical procedures, to a (primarily) cataract practice can be challenging—technically, operationally, and economically. Indeed, between 2016 and 2021, the proportion of respondents to the ESCRS annual Clinical Trends Survey performing glaucoma surgery declined significantly, while a growing proportion offered only medical glaucoma treatment.1
Still, proponents say non-filtering MIGS procedures are a generally low-risk method that may reduce intraocular pressure (IOP) enough to address mild to moderate glaucoma with fewer or no topical medications. Moreover, since they don’t alter the anatomy as much as trabeculectomy, non-filtering MIGS do not preclude later additional MIGS or more invasive procedures, Dr Bellucci said.
Glaucoma specialist Dr Inder Paul Singh noted that five-year data show reduced IOP and medication need—and better quality of life in some cases—with meshwork stenting procedures compared with cataract surgery alone.2
He has used conventional outflow MIGS for select moderate to severe cases to limit fluctuating IOP and delay subconjunctival surgery for those at high risk for complications.
However, glaucoma experts caution that non-filtering MIGS devices may not be suitable, even for patients with mild to moderate glaucoma, if the disease is likely to progress or they need a low-target IOP. And the only way to tell is to follow them for a year or more, said glaucoma specialist Dr Luis Abegão Pinto.
 Complicating the issue are inconsistencies in how trials report data and a lack of large randomised prospective trials to determine efficacy of some MIGS procedures. “We need better data to know what really works,” said Dr Pinto, who co-chairs a task force of the European Glaucoma Society that has developed recommendations for uniform data collection in glaucoma studies.
Complicating the issue are inconsistencies in how trials report data and a lack of large randomised prospective trials to determine efficacy of some MIGS procedures. “We need better data to know what really works,” said Dr Pinto, who co-chairs a task force of the European Glaucoma Society that has developed recommendations for uniform data collection in glaucoma studies.
To the right are some factors to consider when deciding to treat or refer glaucoma patients in a primarily cataract practice.
What to look for
Since many cataract patients have no contact with ophthalmologists until their vision declines, the preoperative workup goal should be to determine why the patient does not see well, including any comorbidities such as glaucoma, Dr Pinto said. Then, any treatment decision—including medical treatment, MIGS, or filtration surgery—should be driven by the treatment goal, though this can be difficult to establish at the first visit. Dr Singh added glaucoma surgery goals also vary by patient, with some requiring lower IOP regardless of eye drop need.
IOP over 20 mmHg is an obvious red flag. Asymmetry between the optic nerve heads in the two eyes is another, Dr Bellucci said. Optical coherence tomography (OCT) helps spot optic nerve head tissue loss. Visual fields are mandatory when any optic nerve damage is evident on OCT, and gonioscopy should be performed if not previously documented.
Dr Pinto stressed doing a complete diagnostic workup rather than relying on OCT, which cannot be the sole source of diagnosis. Visual fields, he noted, are the best way to detect and track progression.
Training for surgeons and staff
As with any new procedure, attend lectures and training, and try MIGS first in wet labs before starting with uncomplicated glaucoma patients, Dr Bellucci said. Learning to accurately identify the trabecular meshwork and where to position bypass devices to be effective is critical, said specialty expert Dr Antonio Maria Fea.
For ophthalmologists out of practise with gonioscopy, fellow specialist Professor Carlo Enrico Traverso recommends first performing intraoperative gonioscopy on a patient who doesn’t need glaucoma surgery. Dr Pinto suggested starting with one or two procedures. “It is impossible to master 10 different technologies with the same proficiency you have in cataract surgery.”
And don’t forget training staff. “There will have to be a certain number of [MIGS] procedures you have to do routinely for the nurse to know the next step to make sure it is as efficient as if you are doing a phaco alone,” Dr Pinto said.
He noted some cataract surgeons are reluctant to adopt even trabecular bypass MIGS because it interferes with cataract surgery efficiency, particularly for those using a superior incision approach. Implanting a stent then requires moving the microscope to a temporal position. “At the end of the day, you’ve probably done two fewer cataracts to account for that time.” Dr Fea added setting aside one day a week for glaucoma patients or moving them to the end of the schedule can help improve efficiency, while Dr Singh said reducing eye drop use with MIGS may save time on follow-up.
Bleb-forming procedures require additional training in managing antimetabolites, ensuring the tube enters the subconjunctival space, and managing complications such as choroidal detachments and fibrosis, Dr Fea said. He recommends following cases closely for the first three to four months after surgery—or even longer if the bleb has to be revised. The period between visits can be extended for uneventful cases, but “I would not leave the patient alone for more than three months for the first two years.”
Treat versus refer
Not all glaucoma patients can be treated without the expertise of a glaucoma surgeon, Dr Bellucci said. He mostly treats patients with early primary open-angle glaucoma who are aware of their condition, but generally refers low-tension glaucoma patients. He also refers patients with significant nerve damage or progression, especially young or myopic patients. Most importantly, he refers advanced glaucoma patients possibly at risk of losing vision permanently due to surgery, known as wipeout syndrome. High myopia, uveitis, secondary glaucoma, and congenital glaucoma, Dr Fea said, should likewise be referred.
Dr Pinto suggests treating patients with whom surgeons have an established relationship. That patient will likely return for follow-up and can be referred if they progress to a glaucoma surgeon with more treatment options, he said.
Combined or separate procedures
MIGS procedures are designed to be used with cataract surgery or alone. But for cases requiring a lower target IOP, filtration procedures, including trabeculectomy and the filtering implants, are better, Prof Traverso said. For these options, the evidence and consensus are for cataract surgery first, followed three months (or more) later by the glaucoma procedure on a quiet eye, is generally easier and yields better results. However, patients with severe disease and very high IOP that cannot be controlled without immediate filtration indicate combined surgery, he added.
Educating patients
 Educating patients on the limitations of glaucoma procedures and the need for lifelong follow-up is essential for good long-term outcomes. Dr Pinto advises having an honest conversation with the patient that does not overpromise or discard the safety concerns. Dr Singh suggests telling the patients, “we are on a journey,” and will use a combination of therapies and technologies to help protect them from losing vision and maintain their quality of life.
Educating patients on the limitations of glaucoma procedures and the need for lifelong follow-up is essential for good long-term outcomes. Dr Pinto advises having an honest conversation with the patient that does not overpromise or discard the safety concerns. Dr Singh suggests telling the patients, “we are on a journey,” and will use a combination of therapies and technologies to help protect them from losing vision and maintain their quality of life.
“You don’t want to say to the patient that he is cured,” Dr Fea said. “I’ve seen patients who forget everything [after glaucoma surgery] and then come back five years later, and they are miserable.”
Above all, follow the Hippocratic oath: do no harm. Whether slowing progression, lowering IOP, or reducing medication burden, know the goal and only do the procedure if it will help the patient, Dr Pinto said.
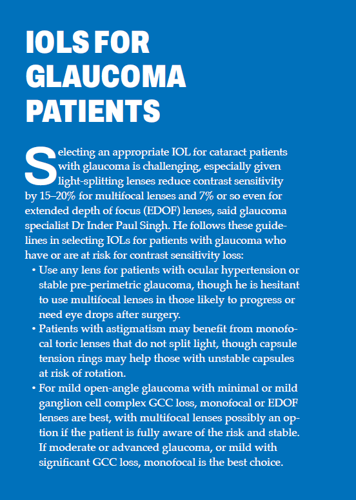
Dr Bellucci largely agreed. In patients with early glaucoma without visual field or nerve loss and low IOP, he will use a multifocal lens and femto-cataract surgery. However, for more advanced cases, he does not do anything to risk an IOP spike, avoiding femtosecond lasers, instead opting for advanced fluidics phaco machines. He also will not place a multifocal lens into an eye with contrast sensitivity already reduced due to glaucoma.
For citation notes, see page 40.
Roberto Bellucci MD is an ophthalmologist in Verona, Italy, and a former ESCRS president. roberto.bellucci52@gmail.com
Luis Abegão Pinto MD, PhD is head of the glaucoma unit and assistant professor of ophthalmology at Lisbon University, Portugal. abegao.pinto@chln.min-saude.pt
Antonio Maria Fea MD, PhD is an ophthalmologist, head of glaucoma at the ocular clinic, and aggregate professor at the University of Turin, Italy. antoniomfea@gmail.com
Inder Paul Singh MD is an ophthalmologist at the Eye Centers of Racine and Kenosha, Wisconsin, US. ipsingh@amazingeye.com
Carlo Enrico Traverso MD is professor and chairman of the Clinica Oculistica, Di.N.O.G.M.I., University of Genoa, Policlinico Ospedale San Martino IRCCS, Italy. mc8620@mclink.it; cet@mclink.it
Latest Articles
From Lab to Life: Corneal Repair Goes Cellular
Long-awaited cellular therapies for corneal endothelial disease enter the clinic.
Balancing Innovation and Safety
Ensuring access to advanced cell therapies amid regulatory overhaul.
With Eyes on Its Future, ESCRS Celebrates Its Past
Winter Meeting offers opportunities to experiment with new concepts and formats.
Best of ESCRS Winter Meeting 2024
Following the New Generation
EDOF IOLs an option for eyes with mild comorbidities, showing potential in mini-monovision strategies.
Refocus on Multifocals
Trifocal IOLs continue to improve as consensus grows regarding indications and contraindications.
Common Myths in Presbyopia Correction
Patient education key to satisfaction with refractive IOLs.
Reversible Multifocality
Two-lens combination offers low-risk spectacle independence for cataract patients and presbyopes.
Managing a Cataract Surgery Refractive Miss
Weighing the pros and cons of options for intraocular intervention.
Unleashing OCT’s Full Potential
Performance of newest tool for corneal evaluation meets or beats older standard technologies.