IOP and the distal drainage tract
New discovery regarding outflow resistance in the aqueous drainage tract has significant treatment implications
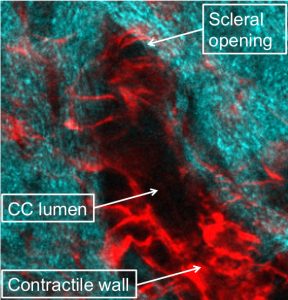
Two-photon image of the collector channel. A significant
proportion of the channel cross-sectional area comprises
wall cells with filamentous actin (red). This leaves a
lumen (black oval) that is smaller than might be expected
relative to the opening in sclera (cyan)
Outflow resistance in the aqueous drainage tract distal to trabecular meshwork is potentially an important determinant of intraocular pressure and success of trabecular bypass glaucoma surgeries, reported James Tan MD, PhD from the Doheny Eye Institute and UCLA in Los Angeles, USA.
Dr Tan addressed delegates during the ESCRS Main Symposium, “Glaucoma for the Cataract Surgeon”, at the 36th annual ESCRS Congress in Vienna. He shared the results of cutting-edge research entitled “Imaging Distal Aqueous Outflow: Mouse Lessons Relevant to Trabecular Bypass Surgery”.
“The distal aqueous drainage tract is denser and much more complex than previously thought. However, we don’t yet have a deep understanding of how this region affects intraocular pressure,” he said.
Conventional wisdom states that the intrascleral outflow tract distal of the trabecular meshwork is low-resistance, allowing nearly unrestricted outflow to the episcleral veins. This would imply that trabecular bypass surgery, such as ab interno trabeculotomy or microstenting procedures, are sufficient to eliminate resistance to outflow. However, the results of Dr Tan’s imaging research suggest otherwise.
“Significant resistance seems to reside in the distal outflow tract beyond the trabecular meshwork,” he said. “This is important for two reasons. First, it might affect intraocular pressure in glaucoma patients. Second, it might affect the results of glaucoma bypass surgery. Understanding this system might allow us to target it pharmacologically.”
The functional organisation and regulation of this tract was previously unknown, and it remains unclear whether disease might affect this system to affect intraocular pressure.
“The complexity of the distal drainage tract had earlier been suggested using OCT virtual casting, and aqueous angiography had shown that the distal outflow pattern is regional and that it varies with time,” said Dr Tan. Further, phase-sensitive OCT had shown that the outflow is pulsatile with the meshwork showing cyclical expansion & contraction in sync with cardiac output.
Dr Tan’s research adds significantly to our knowledge of the tract. In transgenic mice that were engineered to produce fluorescent endothelial proteins, high-resolution two-photon deep tissue optical sectioning showed that the distal tract resembles a vascular system with some features of lymphatic vessels. The mouse aqueous outflow system is known to highly resemble humans’, only smaller.

James Tan MD, PhD
One of the mysteries that Dr Tan sought to unravel was whether the distal tract was a type of vascular system. The first question was: is the distal tract lined with endothelium, and, if so, what type?
“The intrascleral plexus can be shown to be lined by cells, and those in Schlemm’s canal are Prox1-positive, like cells of the lymphatic endothelium,” said Dr Tan. “But Schlemm’s canal endothelium also expresses CD31 and other proteins found in blood vessel endothelium.” This suggests that the endothelium of the aqueous outflow tract carries features of both lymphatic and blood vessel endothelial cells.
On the other hand: “Distal tract walls showed prominent filamentous actin labelling, reflecting cells in a contracted state. Smooth muscle markers were seen in these contractile wall regions, which may have the capacity to affect lumen size,” said Dr Tan. The distal tract’s wall organisation resembles that of blood vessels, and contraction might cause a narrow-calibre, high-resistance system that could significantly decrease outflow.
“In summary, the distal outflow tract has vascular properties with several differences as compared to vessels that carry lymph and blood,” he said. “That it has its own type of endothelium is not surprising because it carries a different type of fluid, aqueous humour.”
Dr Tan believes that the distal outflow tract is not just an inert system of openings. Instead, it is a dynamic system with auto-regulatory properties, which might offer low resistance when relaxed and higher resistance when contracted to a narrow-calibre state.
“Although it is unclear how distal resistance is modulated, this auto-regulation might be a target for IOP-lowering treatment,” he concluded.
Dr Tan also suggested that the distal tract might adapt after a micro-incisional glaucoma procedure, affecting the outcome of surgery.
Authors
Leigh Spielberg
Published
Thursday, March 21, 2019
Category