Astigmatism Debate
Debate highlights optimal strategy to tackle low astigmatism
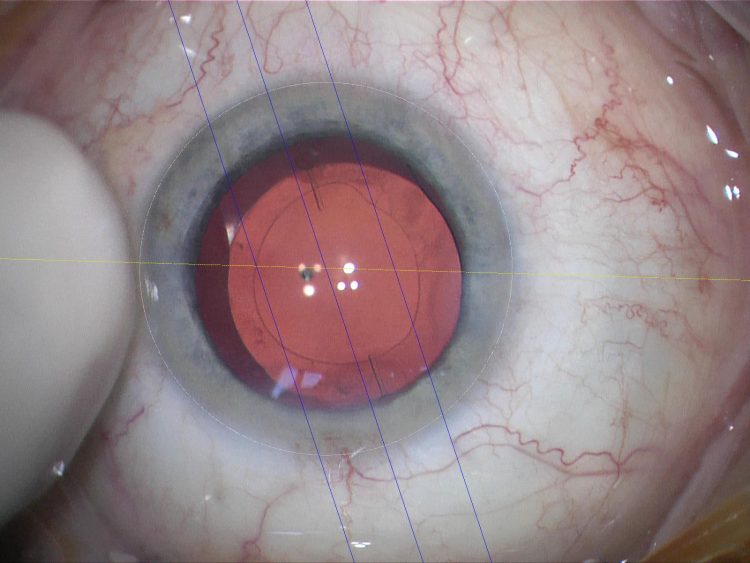 A surgeon’s view through the eyepiece of a toric IOL being alligned with a markerless tracking system (Zeiss Meditec AG, Germany. Courtesy of Oliver Findl MD
A surgeon’s view through the eyepiece of a toric IOL being alligned with a markerless tracking system (Zeiss Meditec AG, Germany. Courtesy of Oliver Findl MDThe question of how best to deal with low level astigmatism in cataract surgery was the subject of a lively debate during the JCRS Symposium held during the XXXII Congress of the ESCRS in London.
Douglas D Koch MD, Cullen Eye Institute, Baylor College of Medicine, Houston, Texas, US, argued the case for femtosecond laser correction as the optimal approach, while Oliver Findl MD presented the arguments in favour of toric intraocular lens (IOL) correction.
Dr Koch said that, in his view, femtosecond laser-assisted cataract surgery (FLACS) represents the best approach currently available for astigmatic correction in cataract surgery.
“The goal of astigmatic correction in general is to reduce astigmatism to 0.5D or less and I think the aim is to correct this simply, safely, efficiently and affordably. The femtosecond laser fulfils all of these criteria and it is available to us now,” he said.
Dr Koch said that there are two types of incision that can be made with the femtosecond laser for astigmatic correction: penetrating astigmatic keratotomy (AK) and non-penetrating intrastromal AK (ISAK).
Dr Koch said his own preference is to use non-penetrating incisions, which entail no wound gape, no risk of infection and no epithelial ingrowth. “One can also theoretically expect less inflammation, quicker visual recovery and enhanced patient comfort with this approach,” he said.
In his own series of patients using the Catalys femtosecond laser (AMO), Dr Koch reported excellent results in 24 eyes of 21 patients using a modified version of a nomogram developed by Julian Stevens MD at Moorfields Eye Hospital, in order to account for posterior corneal astigmatism. In 19 eyes included in the final analysis, 63 per cent had 0.25D or less of manifest cylinder after treatment while almost 95 per cent of patients were 0.50D or less.
Future work with femtosecond incisions will entail better standardisation of the depth of the cuts, evolution of the nomograms and longer-term follow-up, said Dr Koch. He added that the cost factor also works in the laser’s favour.
“Femto laser costs about $850 an eye at a rate of 23 cases per month and $400 an eye once the laser is paid off. A toric IOL costs about $500 an eye and has none of the other advantages of the femto laser such as capsulotomy, lens softening, incisions etc. So the choice is obvious – laser is safe, effective and cheaper in the long-term, and it is faster than aligning a toric IOL at the time of surgery,” he said.
Good definition
Actually, the case for the laser is not so obvious at all, according to Oliver Findl MD, Vienna Institute for Research in Ocular Surgery, Austria.
“The problem we have here is that we do not really have a good definition of low astigmatism. What is clear is that below 0.75D of astigmatism, especially when measured on the cornea, the measurements are so noisy and so variable from method to method and device to device that it is difficult to speak about definite astigmatism,” he said.
Looking at astigmatism correction techniques currently available, Dr Findl said that toric IOLs offer good astigmatism-reducing effect if well aligned and rotationally stable, while opposite clear cornea incisions (OCCIs) and peripheral corneal relaxing incisions (PCRIs) are easy to perform but produce variable results.
Dr Findl noted that PCRIs seem to be so variable in their outcomes because of poor prediction of the corneal response to the incisions and also that the effect fades over time.
“We believe that the reason for this is probably the variability in the viscoelastic properties of the cornea which varies a lot from one patient to the other and also the scarring reaction after surgery which is also very variable. The key point here is that this would also not be very different for FLACS in terms of predicting how the cornea might react, because we are still talking about incisions even if they are made by a laser,” he said.
Looking at outcomes with toric IOLs in 250 eyes of 200 patients, Dr Findl noted that the most unpredictable outcomes were for those patients with low astigmatism.
The reasons for poor astigmatic reduction with toric IOLs stem from factors such as inaccurate preoperative calculations of IOL power and posterior surface of the cornea, as well as intraoperative issues such as mislabelling of the IOL, surgically-induced astigmatism and IOL misalignment, said Dr Findl.
Of these factors, preoperative measurement errors, with large inter-device variability within and between different keratometric measurements and topographic measurements, represent the main source of error, said Dr Findl. Add in diurnal changes in corneal measurements over the course of the day and differences in postoperative refraction measures and it is easy to see why there is so much variability correcting low-level astigmatism, he said.
“There are so many prediction errors for residual astigmatism after toric IOL implantation and most of these factors are not influenced by FLACS at all,” he concluded.
Douglas D Koch: dkoch@bcm.tmc.edu
Oliver Findl: oliver@findl.at
Authors
Dermot McGrath
Published
Thursday, April 2, 2015
Category